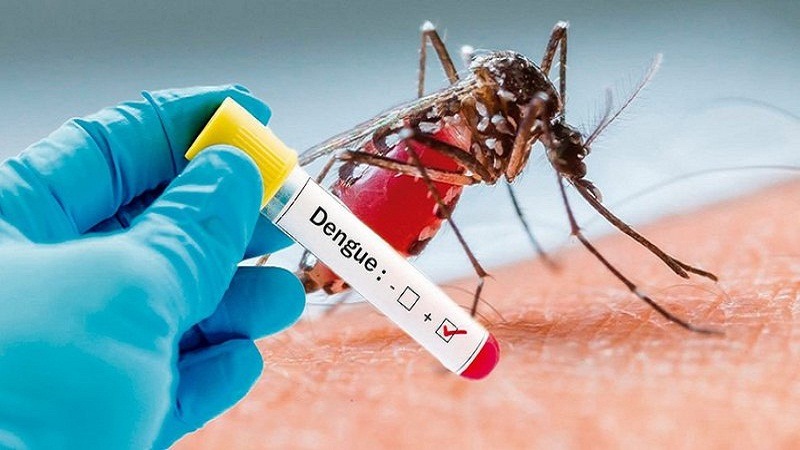
Chikungunya and dengue cases surge as Aedes mosquitoes spread in Kenya
Unlike many other mosquitoes, Aedes mosquitoes are active during the daytime, and they are especially adapted to live in urban and semi-urban environments.
The rapid growth of cities combined with poor water and waste management is creating ideal breeding grounds for mosquitoes, particularly the Aedes species that spread dangerous arboviruses such as dengue, chikungunya, Zika, and yellow fever.
In Kenya, these challenges are already playing out in alarming ways, with recurring outbreaks signalling a worsening public health crisis. The expanding threat is fueled by climate change, which alters rainfall patterns and temperatures, allowing mosquito populations to thrive in areas previously considered low-risk.
More To Read
- African governments urged to boost funding as NCD crisis deepens
- Burkina Faso shuts down Bill Gates-backed mosquito project over safety, ethical concerns
- US suspends chikungunya vaccine after reports of severe side effects
- Kenya records landmark milestones in fight against HIV, malaria, TB and sleeping sickness
- Kamukunji faces vaccine crisis as over 12,000 children miss routine immunisation
- Breeding grounds for danger: How improper waste management drives disease transmission
According to the Centre for Disease Control (CDC), Aedes mosquitoes are small, dark-colored, with distinctive white markings on their legs and bodies. Two of the most common species, Aedes aegypti and Aedes albopictus, are known for their ability to transmit serious and sometimes life-threatening diseases. Unlike many other mosquitoes, Aedes mosquitoes are active during the day and are adapted to urban and semi-urban environments.
What makes Aedes mosquitoes particularly dangerous is their role as vectors of several major diseases, including dengue fever, Zika virus, chikungunya, and yellow fever. These illnesses can cause a range of symptoms such as high fever, severe joint and muscle pain, rashes, and in some cases, complications like internal bleeding, birth defects, or even death.
One of the most critical factors contributing to the spread of Aedes mosquitoes is stagnant water. They lay their eggs in still water, and even small amounts—such as water collected in flower pots, old tires, or open containers — can serve as ideal breeding sites. Eggs laid by Aedes mosquitoes are remarkably resilient and can survive for months in dry conditions, hatching as soon as they come into contact with water.
Poor water management plays a major role in encouraging mosquito breeding. When communities lack proper drainage, leave water containers uncovered, or allow rainwater to collect in discarded items, they unintentionally create environments where Aedes mosquitoes can thrive. The combination of stagnant water and inadequate sanitation practices turns urban areas into hotspots for mosquito-borne disease outbreaks.
Coastal cities like Mombasa, Lamu, and Kilifi have long grappled with dengue and chikungunya outbreaks. However, more recent studies have revealed the presence of Aedes mosquitoes in Nairobi’s informal settlements—places historically thought to be less hospitable to these vectors due to cooler, higher-altitude climates. This expansion is attributed to rising temperatures and unpredictable rainfall, both linked to climate change.
Between 2019 and 2022, Kenya reported several significant chikungunya outbreaks, with hundreds of confirmed cases, while dengue cases have steadily increased in coastal counties. Informal settlements bear the brunt of these epidemics. Poor drainage systems, accumulation of stagnant water in discarded containers, and inconsistent access to piped water create numerous breeding sites for mosquitoes.
A 2022 study published in PLOS Neglected Tropical Diseases found that over 60 per cent of households in Kenya’s urban informal settlements lacked adequate waste management and a reliable water supply, forcing residents to store water in uncovered containers that facilitate mosquito reproduction.
The health impacts are profound. While arboviruses generally have lower mortality rates than some other infectious diseases, the symptoms—fever, severe joint pain, rash, and fatigue—can be debilitating, often lasting for weeks or months. Many infected individuals miss work or school, leading to economic losses for families and communities.
Health facilities in affected areas experience surges in patient visits during outbreaks, straining resources and complicating care delivery. The similarity of arbovirus symptoms to malaria, which is endemic in Kenya, often results in misdiagnosis, hindering timely treatment and outbreak control.
Beyond the immediate health toll, long-term consequences include chronic joint pain and arthritis-like conditions for some chikungunya patients, significantly reducing their quality of life and ability to work. These impacts reverberate through communities, especially in informal settlements, where access to healthcare is limited and economic resilience is low.
Kenya has made efforts to address this growing challenge. The Ministry of Health (MoH) has integrated arbovirus surveillance into its disease monitoring systems and launched community education campaigns promoting the elimination of standing water and proper waste disposal.
Pilot programs in Mombasa have shown promise, reducing mosquito populations by as much as 40 per cent during peak seasons through larvicide application and community engagement. However, scaling such initiatives remains difficult amid rapid urban growth and limited resources.
Over one billion people in Africa live in environments increasingly suitable for Aedes mosquitoes, with countries like Sudan, Nigeria, Tanzania, Ethiopia, and Mozambique reporting major arbovirus outbreaks. In 2023, Mozambique recorded over 10,000 chikungunya cases, while Sudan faced one of its worst dengue epidemics recently. The World Health Organisation (WHO) warns that by 2080, up to 70 per cent of Africa’s population could be at risk of dengue, driven by urbanisation and climate change.
Globally, an estimated 5.6 billion people — nearly 70 per cent of the world’s population—now face increased exposure to mosquito-borne diseases. Regions in South America, Southeast Asia, and parts of the United States are also witnessing rising outbreaks and longer transmission seasons.
Among the three diseases, Chikungunya has been the most prominent in Kenya. The country first experienced a major outbreak in Mandera County in 2016, where nearly 1,800 cases were reported within just over a month. Though this outbreak predates the last five years, it set the stage for continued virus activity.
Another significant wave occurred in Mombasa between late 2017 and early 2018, when hundreds of suspected cases were reported across multiple sub-counties. This outbreak was notable not only for its size but also for the co-infections with dengue fever, suggesting that both viruses were circulating at the same time—a situation made more dangerous by the difficulty in distinguishing the two illnesses without laboratory testing.
Chikungunya returned to the spotlight in June 2025, when a new outbreak emerged again in Mombasa. Tests by the Kenya Medical Research Institute (KEMRI) confirmed 25 new cases. The outbreak was attributed to recent heavy rains, which led to widespread water stagnation in urban areas.
In response, local health authorities launched an aggressive mosquito-control campaign that included fumigation, public awareness drives, and clearing of blocked drainage systems. This outbreak underscored how vulnerable urban centres remain to mosquito-borne illnesses, especially during Kenya’s rainy seasons.
In addition to these coastal outbreaks, a 2024 study in the Mt Elgon region, in western Kenya, revealed that the chikungunya virus is also circulating in inland areas.
Blood samples taken from patients with fever symptoms showed that nearly 10 per cent had antibodies to the virus, suggesting that many people had been exposed to chikungunya without being officially diagnosed. This finding is important because it indicates that chikungunya may be more widespread than previously thought, especially in regions with limited access to healthcare and diagnostic tools.
While not as dominant as Chikungunya in Kenya, dengue fever has consistently appeared in the same regions and under similar conditions. Coastal counties such as Mombasa, Kilifi, Wajir, and Mandera remain at risk, particularly during the rainy seasons when mosquito populations surge.
During the 2017–2018 chikungunya outbreak in Mombasa, some patients tested positive for dengue, reinforcing the close link between the two diseases. Although there have been no massive dengue outbreaks in Kenya in recent years, sporadic cases and small clusters continue to occur, often going unreported or undiagnosed due to limited testing facilities.
There have been no major outbreaks of Zika virus and only rare or isolated cases, if any, in the last five years.
Nevertheless, Zika virus is also transmitted by Aedes mosquitoes and has caused serious health emergencies in other parts of the world, including birth defects and neurological conditions.
Top Stories Today










































