45 more health facilities to be deregistered as ministry uncovers widespread fraud in hospitals
The CS cited examples, including Nabuala Hospital in Bungoma, which falsified claims for multiple Caesarean sections on the same patient within days, Kotiende Medical Centre in Homa Bay, where one individual signed off for both day and night shifts across consecutive days and Vebeneza Medical Centre in Nairobi, which converted outpatient visits into inpatient admissions and routinely admitted its own employees.
A total of 45 more health facilities across the country will be degazetted for fraudulent practices as the Ministry of Health steps up its anti-fraud campaign.
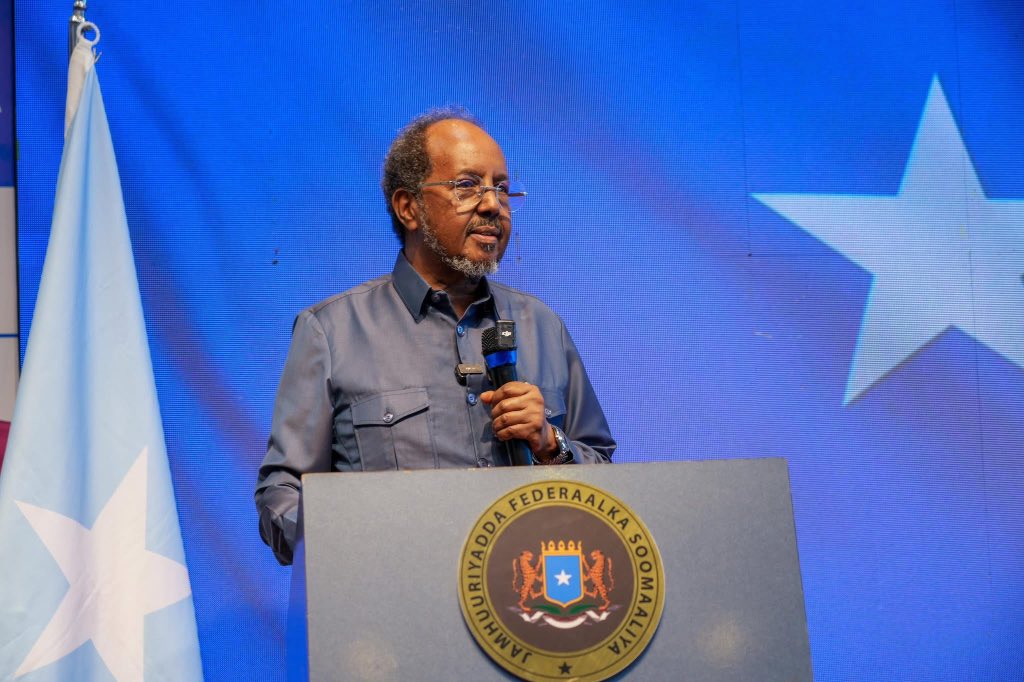
Addressing the media on Monday at Afya House, Nairobi, Health Cabinet Secretary Aden Duale said the ongoing crackdown has uncovered rampant malpractice, including upcoding, falsifying records, converting outpatient visits into inpatient claims and billing for non-existent patients.
More To Read
- Ministry of Health clears 7,414 UHC workers for government payroll as 215 ghost staff removed
- RUPHA raises alarm as ghost hospitals siphon millions of shillings in SHA claims
- Silent crisis of self-medication and gaps in SHA services for patients with chronic illnesses
- SHA denies wiring Sh20 million to ghost hospital in Homa Bay, confirms payment to Nyandiwa Level 4
- Over 700 private hospitals face collapse as SHA, NHIF debts hit Sh76 billion
- Hospitals get Sh3.4 billion boost as SHA settles insurance claims
He said these will add to the 40 facilities recently suspended by the Social Health Authority (SHA), alongside 728 already closed and 301 downgraded by the Kenya Medical Practitioners and Dentists Council.
He noted that his ministry has taken a zero-tolerance approach since he assumed office in April, with a new digital system designed to detect and eliminate the loopholes that crippled the defunct National Health Insurance Fund (NHIF).
“The primary function of our digital system is to detect fraud. We have seen that facilities are looking for innovative ways to cheat the system, but our digital architecture is designed to detect and flag anomalies at every stage of the claims process,” he said, adding that the artificial intelligence module has become more effective as more data is collected.
“Hence, you will find that fraud can be detected and stopped at any point, including at the payment stage.”
He revealed that forensic audits had exposed troubling practices such as unsupported maternity claims, fabricated clinical records, suspicious admissions of staff as patients and claims filed for patients simultaneously admitted in multiple hospitals.
The CS cited examples, including Nabuala Hospital in Bungoma, which falsified claims for multiple Caesarean sections on the same patient within days, Kotiende Medical Centre in Homa Bay, where one individual signed off for both day and night shifts across consecutive days and Vebeneza Medical Centre in Nairobi, which converted outpatient visits into inpatient admissions and routinely admitted its own employees.
He also pointed to Jambo Jipya Hospital in Mtwapa for submitting a fraudulent claim for a Caesarean section where a normal delivery had occurred, and New Manyalo Nursing Home in Wajir for converting numerous outpatient cases into inpatient claims beyond its bed capacity, while admitting patients already listed in other facilities.
In Mandera, facilities including Al-Masry Nursing Home, Rhamu Dimtu Medical Centre, Balanga Medical Centre, Care Connect Hospital, Al Shamsi Medical Centre, Merti Nursing Home, Zamzam Nursing Home and Nibil Nursing Home were found to have colluded to submit 312 fraudulent claims for patients allegedly admitted to multiple facilities on the same dates.
“To all healthcare providers: consider this a final warning. We are watching. Any facility, doctor, or patient found to be involved in fraudulent activities will be held liable and face the full force of the law. We’ve already initiated the process to recover paid monies and will involve law enforcement to prosecute perpetrators,” he warned.
He called on the public to support the government’s anti-fraud campaign by reporting malpractice to the SHA through the toll-free number 147.
“Please work with us to ensure that every cent of public money is used prudently for its intended purpose: to provide legitimate, quality healthcare to all. Your participation is vital in protecting our social health insurer and securing a healthier future for our nation,” he said.
Duale also reaffirmed the ministry’s commitment to transparency, noting that lists of all health facilities paid by SHA are published regularly, even though there is no legal requirement to do so. He stressed that this approach ensures accountability and allows Kenyans to monitor how public funds are being spent.
SHA claims
Providing an update on claims since the rollout of the Taifa Care programme in October 2024, Duale said health facilities had submitted claims worth Sh9 billion under the Primary Healthcare (PHC) programme, of which Sh7.7 billion had already been paid, with the balance scheduled for the next cycle.
Under the Social Health Insurance Fund (SHIF), facilities submitted Sh82.7 billion in claims, of which Sh53 billion had been paid, Sh6.4 billion approved and awaiting payment, Sh10.6 billion rejected due to fraudulent or non-compliant activities, Sh3 billion under re-evaluation for missing documents, Sh2.1 billion under surveillance for further investigation, and Sh7.6 billion for the month of August currently under review.
“This rigorous process is a key part of the Authority’s function under Section 35(2) of the Social Health Insurance Act, 2023, which mandates the Claims Office to review, process, and validate medical claims and conduct quality assurance surveillance,” he said.
On the matter of NHIF’s legacy debt, the CS said the government will honour only verified claims in line with constitutional provisions and financial laws.
“As committed by the President, the government will pay all verified claims of Sh0–10 million. These payments will be factored into the supplementary budget in full respect of the Constitution and relevant financial acts. However, claims above this threshold must still undergo a rigorous verification process,” he said.
“We have a duty to pay only for services legitimately rendered in full respect of Article 201 of the Constitution on the principles of public finance, as well as the Public Finance Management Act and the Social Health Insurance Act, 2023.”
The CS also clarified that SHA contracts directly with individual healthcare facilities and not associations, in line with Section 34 of the Social Health Insurance Act, 2023. He said that while associations such as the Rural & Urban Private Hospitals Association of Kenya (RUPHA) play an important role, the legal responsibility lies with the contracted facilities.
“Our primary obligation is to pay for genuine claims and to protect public money. Therefore, all obligations and accountability vest with the contracted parties—the individual facilities and the SHA. It is the responsibility of each facility to adhere to its contractual and ethical obligations,” he said.
He further disclosed that on August 18, he met the chief executives of major insurers, including Jubilee Health Insurance, AAR Insurance and Old Mutual, to establish a Joint Anti-Fraud Action aimed at bridging financial gaps and strengthening oversight.
“Our strategy is to build a robust, corruption-proof system. I want to be clear: our work has just begun. We will not rest until every Kenyan has access to quality, affordable, and dignified healthcare, free from the burden of fraud,” Duale said.
Top Stories Today