The rising threat of multidrug-resistant tuberculosis in Kenya
Kenya is among the 30 high-burden TB countries worldwide, highlighting the severity of the disease in the region.
The rise in multidrug-resistant tuberculosis (MDR-TB) cases in Kenya has become a serious public health concern, with only two in five patients receiving treatment. This leaves the majority at risk and contributes to the continued spread of the disease.
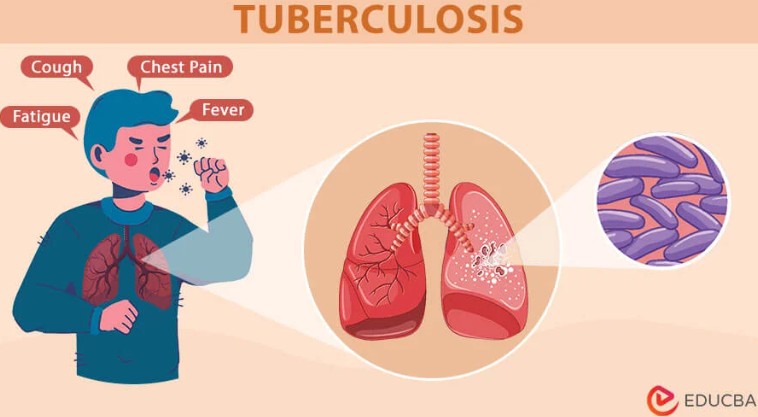
Tuberculosis (TB), caused by the bacterium Mycobacterium tuberculosis, primarily affects the lungs but can also impact other parts of the body, including the brain, spine, and kidneys. It spreads through the air when an infected person coughs, sneezes, or talks. While TB is curable with timely and proper treatment, it remains a significant global health challenge.
More To Read
- Kenya unveils advanced bronchoscopy programme at KNH to strengthen respiratory care
- New antibiotic outperforms standard tuberculosis treatment in global trial
- Tuberculosis cases fall for first time since pandemic- WHO
- Turkana County, Amref launch final phase of HIV, TB and reproductive care project
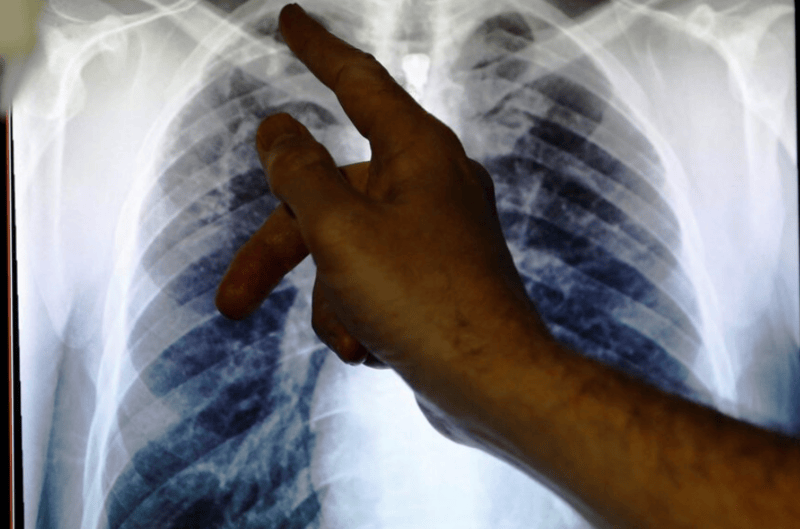
- Kenya rolls out AI-powered chest x-rays to boost early TB detection
- Meet Tanzania’s ‘hero rats’ trained to detect landmines, TB and earthquake survivors
Kenya is among the 30 high-burden TB countries worldwide, highlighting the severity of the disease in the region. Despite progress in detection and treatment, major challenges persist. In 2023, the country recorded 223 TB cases per 100,000 people, signalling an escalating crisis. That same year, TB claimed 32,000 lives in Kenya alone.
Globally, tuberculosis remains a leading infectious killer, with approximately 1.25 million deaths reported in 2023. Among these, 161,000 were individuals also living with HIV, further complicating treatment and management efforts.
The standard TB treatment lasts six months, but the duration may vary depending on the type of TB and the patient’s response to medication. While some patients adhere to their prescriptions and clinic visits, treatment defaulting remains a major challenge in Kenya.
Dr. Esther Mwaura from Nairobi notes that the continued rise in TB cases continues to be primarily driven by stigma, especially among individuals attempting to reintegrate into their communities. This stigma often discourages patients from adhering to their treatment plans or taking the necessary precautions, which complicates efforts to control TB.
The stigma surrounding the disease is characterized by fear, discrimination, and social isolation, with many people associating TB with poor hygiene, poverty, or its contagious nature. This leads to shame and a reluctance to seek treatment.
As a result, patients may abandon their medication or fail to complete the full course, unknowingly contributing to the development of drug resistance. The fear of social exclusion and ostracism often prevents individuals from following their treatment regimen, further hindering TB control and accelerating the spread of resistant strains.
“When TB patients start treatment and begin to feel better, many neglect basic precautions such as covering their mouths when coughing, maintaining proper hygiene, or adhering to dietary guidelines. Due to stigma, some also interact with others without taking necessary precautions, increasing the risk of transmission.”
She explains that since TB is airborne, a patient who does not take the necessary precautions can easily spread the disease to others. Another major challenge contributing to drug resistance is the failure to strictly follow the prescribed treatment regimen.
"TB medication should never be skipped throughout the entire treatment period. Some patients also ignore the recommended timing, taking the drugs inconsistently, which accelerates resistance.”She highlights that adhering to the correct dosage schedule is crucial in preventing drug resistance and ensuring effective treatment.
Dr. Mwaura points out that some patients miss clinic visits, unknowingly developing drug resistance. As a result, they complete their medication only to discover they are still infected or have been reinfected. The side effects of TB treatment, including changes in taste and discomfort, often lead some to abandon treatment entirely, increasing the risk of spreading the disease.
"To prevent drug resistance and avoid weakening the immune system—since prolonged medication can make the body vulnerable to other infections—TB patients should strictly follow their treatment, attend clinic visits, take medication on time, eat a balanced diet, maintain proper hygiene, and most importantly, protect those around them," she advises.
Antibiotics misuse
Multidrug-resistant tuberculosis in Kenya is fueled by incomplete treatment, misuse of antibiotics, and limited access to adequate healthcare. Many patients, feeling better early in their treatment, discontinue their medication, allowing the bacteria to develop resistance. Delayed diagnoses, overcrowded living conditions, and the stigma surrounding the disease further exacerbate its spread, preventing many from seeking necessary care.
The consequences of MDR-TB are profound: it results in higher mortality rates, longer, more costly treatments, and places immense strain on the healthcare system. Social and economic impacts are also significant, as patients are often unable to work, contributing to financial hardship, while the healthcare system is overwhelmed by the rising number of cases.
The World Health Organization highlights that people infected with TB often don’t feel sick and are not contagious. Only a small percentage of those who are infected will develop TB disease and experience symptoms, with babies and children being particularly at higher risk.
TB disease happens when the bacteria multiply and affect different organs in the body. For many, the symptoms are mild and may last for months, making it easy to unknowingly spread the disease to others. Some individuals with TB may not have any symptoms at all.
Common signs of TB disease include a persistent cough, which may sometimes be accompanied by blood, along with chest pain, weakness, fatigue, and weight loss. Additionally, individuals may experience a fever and night sweats. These symptoms often develop slowly, making it easier for the disease to spread without being detected.
It is important to seek medical attention if experiencing symptoms such as a prolonged cough, fever, or unexplained weight loss. Early treatment for TB can prevent the spread of the disease and significantly improve the chances of recovery.
Individuals at higher risk, such as those living with HIV or in close contact with people who have TB at home or work, should get tested for TB.
TB preventive treatment (TPT) helps prevent the infection from developing into TB disease. If prescribed, it is crucial to complete the entire course of TPT.
For individuals with TB, practising good hygiene is essential to prevent transmission. This includes wearing a mask, covering the mouth and nose when coughing or sneezing, avoiding close contact with others, and properly disposing of sputum and tissues.
In healthcare settings and other institutions, special precautions such as the use of respirators and proper ventilation are vital in reducing the risk of TB transmission.
When tuberculosis (TB) does not respond to standard antibiotics, it is categorized as drug-resistant TB, which requires alternative treatments. While TB primarily affects adults in their most productive years, people of all ages are susceptible. More than 80% of TB cases and related deaths occur in low- and middle-income countries. Drug resistance continues to be a significant challenge, with The Lancet projecting that, by 2050, 39 million people will die globally from antimicrobial resistance (AMR), underscoring the growing danger posed by resistant infections.
TB is treated with specific antibiotics, and it is essential for both TB infection and disease. The most commonly prescribed antibiotics include isoniazid, rifampicin, pyrazinamide, and ethambutol. To ensure effectiveness, these medications must be taken daily for 4 to 6 months. Stopping the medication prematurely or without medical advice can be risky, as it may cause the TB bacteria to become resistant to the drugs.
The Ministry of Health in Kenya has outlined a comprehensive plan to tackle drug-resistant tuberculosis (TB) through several key strategies. These include expanding access to early detection and diagnostic services, particularly in underserved areas, to ensure that TB cases are identified promptly. The Ministry is working to improve treatment adherence by providing education and support to patients, encouraging them to complete their full course of treatment, and reducing the risk of resistance. For those with multidrug-resistant TB (MDR-TB)
Top Stories Today