MPs push for annual revisions of SHIF limit to address medical gaps

The limit for optical services is set at Sh1,000 per family per year, with eligibility restricted to children under 18 years.
Members of Parliament have called for regular, annual and timely reviews of the coverage limits under the Social Health Insurance Fund (SHIF) to ensure that patients can access the medical services they need.
Concerns have been raised over the limitations of coverage, particularly for renal and dental care, with lawmakers arguing that the current caps are insufficient compared to the actual costs at medical facilities.
More To Read
- Government to review SHA packages amid calls for better cancer care
- Teachers’ Unions demand clarity as TSC plans to move 400,000 educators to state health scheme
- SHA failing patients with cancer and chronic illnesses, parliamentary report reveals
- Accountants raise concerns after whistleblower loses job at SHA
- Government to enrol all prisoners in SHA by December to combat disease outbreaks
- Religious leaders demand release of SHA funds to hospitals, warn patients’ health is at risk
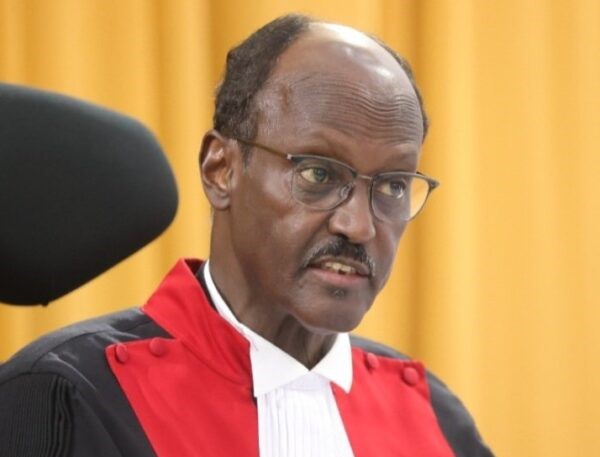
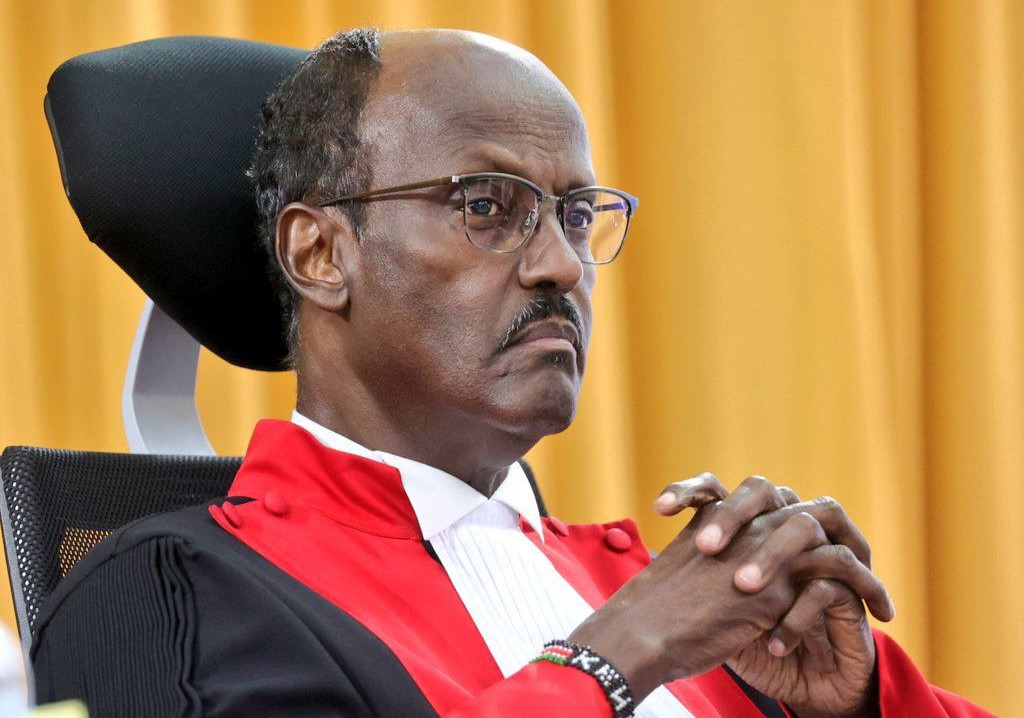
Harry Kimtai, the Principal Secretary of Medical Services, shared the existing coverage limits for various medical services under SHIF on Monday before the MPs.
The limit for optical services is set at Sh1,000 per family per year, with eligibility restricted to children under 18 years.
For dental care, the cap stands at Sh2,000, while essential outpatient services, which include laboratory tests, imaging, prescription medication, and counselling, are capped at Sh900 per beneficiary.
Additionally, normal delivery and essential newborn care are capped at Sh10,000, while a Caesarean section and newborn care are covered up to Sh30,000.
Renal care therapies such as haemodialysis are covered at Sh10,650 per week, while peritoneal dialysis is covered at Sh85,200 per month. Patients must pay any additional costs beyond these limits.
Nyeri Town MP Duncan Mathenge raised concerns about the adequacy of the current dental and optical limits.
He questioned whether Sh2,000 was enough to cover dental care needs, noting that it only accounts for tooth extraction.
"For dental care, the cap is Sh2,000 per year, which only covers tooth extraction. This is unacceptable because modern dentistry focuses on saving teeth rather than extractions," Mathenge said.
Overseas treatment
Mathenge also raised the issue of patients being referred to hospitals in India for overseas treatment, alleging possible collusion between ministry officials and Indian hospitals.
"Mr. PS, explain why patients are being directed to specific hospitals facilitated by SHA. My mother required endocrine services, and despite requesting treatment at a different hospital, we were denied. We had to pay out of pocket to take her to a hospital of our choice," Mathenge lamented.
Robert Pukose, the Committee Chair, also questioned the rationale behind the Sh1,000 cap for optical care and who is responsible for selecting hospitals for Kenyans seeking treatment abroad.
"Who is in charge of empanelling these hospitals? We do not want a situation where ministry officials collude with hospital administrators to create preferential arrangements," he said.
Kitutu Chache South MP Anthony Kibagendi raised concerns over delays in forming review committees, accusing the PS of frustrating patients in need of overseas treatment.
"I am not convinced that SHA is functioning as intended. In reality, SHA is frustrating patients who need medical treatment abroad," Kibagendi argued.
Mogotio MP Reuben Kiborek also expressed his concerns about the Sh500,000 cap for overseas treatment, stating it is insufficient for specialised medical services.
Seme MP James Nyikal emphasised the need for the SHIF cover limits to be reviewed annually to reflect actual medical costs and market rates.
Meanwhile, the country's ongoing financial constraints have left patients seeking treatment for chronic and critical illnesses in public hospitals to pay out of pocket, as healthcare services at level two to level six hospitals continue to be disrupted.
PS Kimtai acknowledged that SHIF is currently only partially operational, with coverage limited to emergency services for the first 24 hours after a patient's admission.
"The fund provides coverage for urgent care, resuscitation, and stabilisation for specific emergency services as outlined in the Gazetted benefit package," Kimtai said.
Partial activation
However, he noted that the chronic and critical illness components of SHIF have not yet been activated due to budgetary constraints.
Although the transition from the National Health Insurance Fund (NHIF) to SHIF took place in October 2023, services for chronic and critical illnesses were only partially activated in December, beginning with emergency care in level five and six hospitals.
Tracy John, the acting director for benefits and claims management, explained the delays.
"The system for these specific services was only activated in December, starting with level five and six hospitals. As a result, claims only began coming in at the end of December," she said.
Anthony Lenaiyara, CEO of the Digital Health Agency, reported that, as of January, 21.6 million claims had been submitted under the fund, which received Sh2 billion in the current financial year.
This includes cases such as cardiac arrest, trauma, and other major health conditions.
Lenaiyara noted the increasing strain on the healthcare system caused by the funding gap.
The MPs and health experts agree that timely and transparent reviews of SHIF cover limits are essential to ensuring all Kenyans can access quality and affordable healthcare.
Top Stories Today