SHA failing patients with cancer and chronic illnesses, parliamentary report reveals

Despite being operational for over a year, SHA continues to face recurring operational and policy problems that are overwhelming healthcare providers.
Kenya’s Social Health Authority (SHA) is struggling to provide basic healthcare services, leaving patients with serious illnesses, including cancer and kidney disease, waiting longer for treatment, a parliamentary report has revealed.
Presented last Tuesday by the National Assembly Departmental Health Committee, the preliminary findings show that teenage mothers, infants, and people with chronic conditions are among those most affected.
More To Read
- TSC confirms shift to SHA cover for teachers from December 1
- TSC sued over teachers’ migration from MINET insurance to SHA
- 1,567 injured police officers compensated, says Mwangangi as Senate pushes for transparency
- SHA announces refund process for mistaken M-Pesa premium payments
- Ruto announces increase in cancer treatment cover to Sh800,000 under SHA from December 1, 2025
- Government to review SHA packages amid calls for better cancer care
Despite being operational for over a year, SHA continues to face recurring operational and policy problems that are overwhelming healthcare providers.
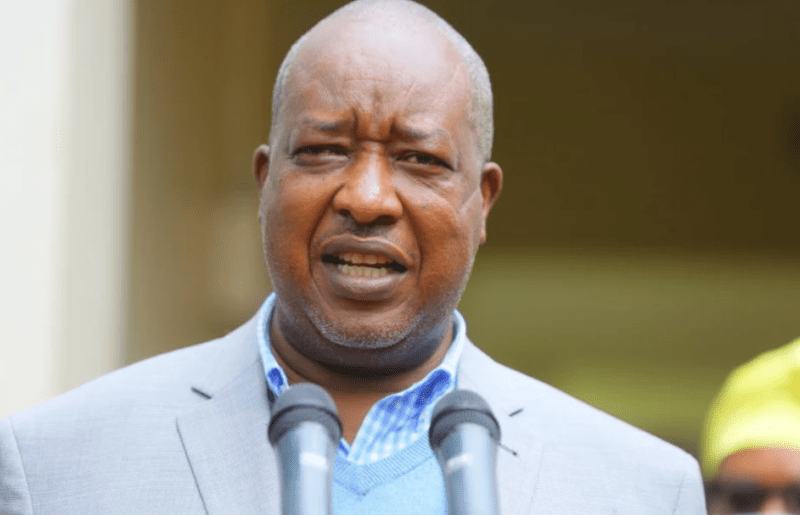
A fact-finding visit to 10 hospitals identified 19 core failures, with cancer patients suffering the greatest impact. “Certain essential diagnostic and follow-up tests are not covered, forcing patients to shoulder high out-of-pocket costs,” said committee chairman and Seme MP James Nyikal.
“Considering the long-term and expensive nature of cancer care, this gap increases the risk of treatment discontinuation, poor outcomes and inequity in access,” he emphasised.
The report also found that the five-day window for laboratory tests and 12-day ICU limits are unrealistic.
Many SHA benefit packages, including Sh30,000 for caesarean sections and restricted outpatient services at Level 5 facilities, do not reflect actual costs, discouraging hospitals from offering specialised care and affecting service quality.
Thousands of disadvantaged Kenyans remain excluded due to the absence of a clear national policy for enrolling indigent patients.
“Teenage mothers without IDs face registration barriers that deny them and their infants access to essential maternal and child health care services,” Nyikal noted.
Other vulnerable groups, including prisoners and chronically ill patients, experience inconsistent coverage. SHA has yet to implement transparent testing methods under Section 27 (2) (c) of the SHA Act, hindering the country’s Universal Health Coverage goals. Requiring annual lump-sum premium payments has also limited access for the poor.
SHA system outages, which occur up to four times per month, disrupt hospital services, while biometric verification presents barriers for patients without IDs, the elderly, or those with faint fingerprints.
Health Cabinet Secretary Aden Duale downplayed these issues, saying the system operates at “95 per cent stable optimum” and added, “We have 147 call centres run by Safaricom. There are minor challenges on the biometric system,” noting technology has reduced staff from 1,800 to 815.
Financial strain is another major problem. Nyeri County Referral Hospital lost over Sh16 million to a neighbouring private hospital due to SHA payment processing errors, and recovery remains stalled. Hospitals have faced delayed and withheld reimbursements, with some months receiving zero payments.
St Elizabeth Swindon Hospital in Kisumu County had to suspend admissions after being misclassified as having “zero beds.”
“Critical service gaps were also noted, including the absence of Neonatal Intensive Care Units (NICUs) in referral hospitals, coupled with shortages of oxygen, essential drugs and utilities during delayed reimbursements,” the report stated.
Unresolved debts from the former National Health Insurance Fund continue to affect hospital operations.
“The Committee noted the lack of transparency in the SHA payment system as reimbursements are often issued as lump sums without clear disaggregation by fund type, hindering effective tracking,” the MPs said.
High claims rejection rates persist despite complete documentation due to missing complaint procedures and unclear resubmission mechanisms, delaying feedback beyond the 90-day statutory period.
Overreliance on Artificial Intelligence without human checks has resulted in unjust claim denials. SHA has not operationalised the Disputes and Resolution Tribunal as legally required, leaving providers without proper redress channels.
Hospitals unable to pay staff for months face strikes and low morale. Among “urgent arrears,” Sh19.2 million owed to St Mary’s Mumias threatens hospital operations and staff retention.
Delays and shortages by the Kenya Medical Supplies Authority (Kemsa) worsen the situation, with some facilities reporting stock levels as low as 30 per cent.
“The resulting stockouts of drugs, oxygen, and critical consumables have compromised patient care and contributed to preventable deaths,” the report warned.
Top Stories Today