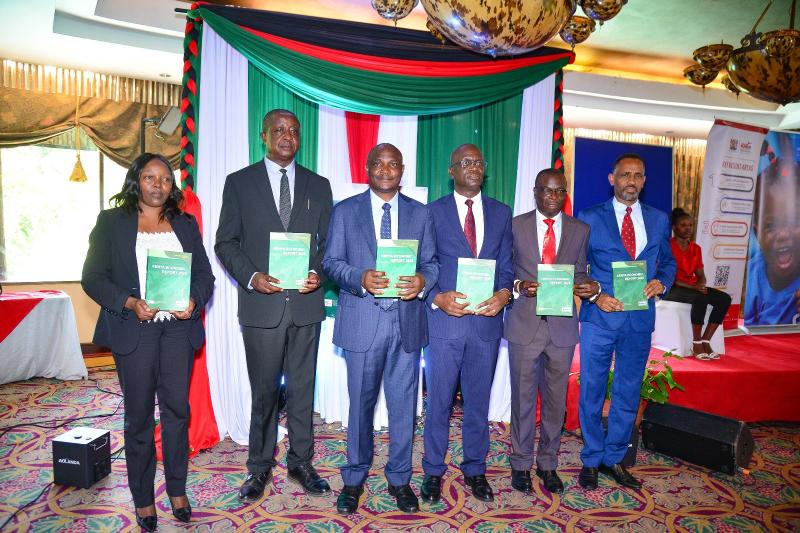
Kenya adopts new WHO HIV testing strategy to boost diagnosis accuracy

Kenyans will thus have their blood tested on three different kits once the rollout is complete.
Starting July 1, Kenya will implement the World Health Organisation's recommended three-test HIV diagnosis strategy, replacing the two-test approach used for the past 15 years.
The three-test strategy comprises three consecutive reactive tests for a positive diagnosis. Kenyans will thus have their blood tested on three different kits once the rollout is complete. Results will be issued after all three tests to ascertain the patient's status.
More To Read
- The hidden stress culprit: How your daily diet is secretly wrecking your mood
- WHO warns of fake breast cancer drug in Africa, Middle East
- WHO review finds no link between childhood vaccines and autism
- Traditional medicine is now a global reality: WHO
- WHO warns tobacco use threatens fertility in men, women
- Out-of-pocket medicine costs surge amid drug shortages in Kenya
This new strategy aims to enhance diagnostic precision and ensure HIV testing adheres to the five C's: voluntary consent, confidentiality, counselling, correct results, and linkage to care.
Conversely, the two-strategy HIV testing approach refers to two distinct methods used to enhance the detection and diagnosis of HIV. These strategies are screening tests: The first step involves using an initial test to detect possible HIV infections. These tests, like rapid tests or ELISAs, look for HIV antibodies or antigens. They are very sensitive and give quick results.
Confirmatory Tests: If the first test is positive, a second, more specific test is done to confirm the diagnosis. This test is usually a Western blot or an HIV-1/HIV-2 differentiation immunoassay. These tests help reduce false positives and ensure the diagnosis is accurate.
WHO warns that a false-positive diagnosis leads to unnecessary lifelong antiretroviral therapy (ART) and social and emotional consequences for clients and their families. A false-negative diagnosis means that someone living with HIV will not benefit from ART and could unknowingly transmit HIV to partners and, in the case of pregnant and breastfeeding women, to their infants.
In Kenya, over 9 million HIV tests are conducted annually across 8,851 testing centres. The Ministry of Health notes the country's commitment to fighting HIV/AIDS, with approximately 1.4 million people currently living with the disease.
As of December 2023, over 1.3 million individuals were receiving treatment at 3,752 facilities nationwide.
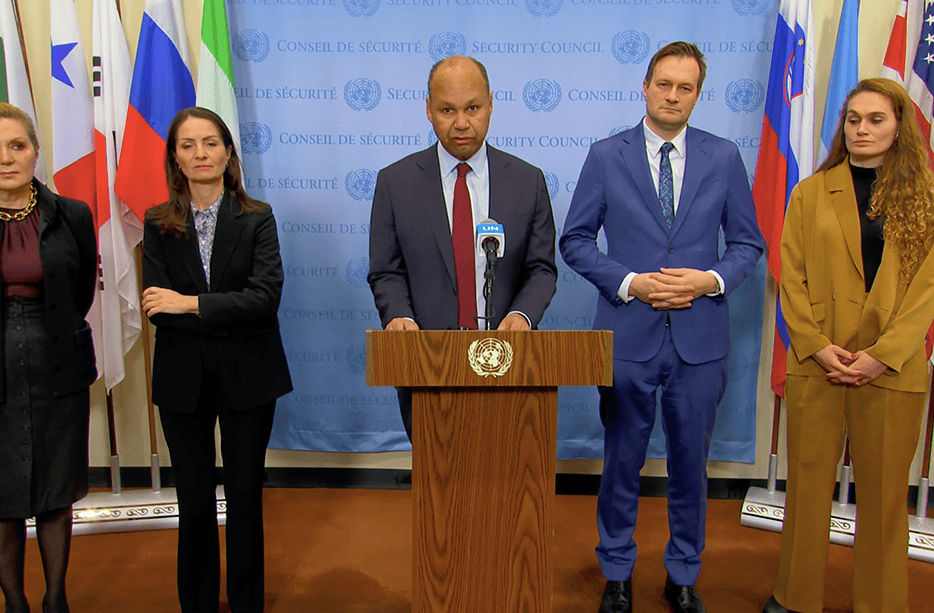
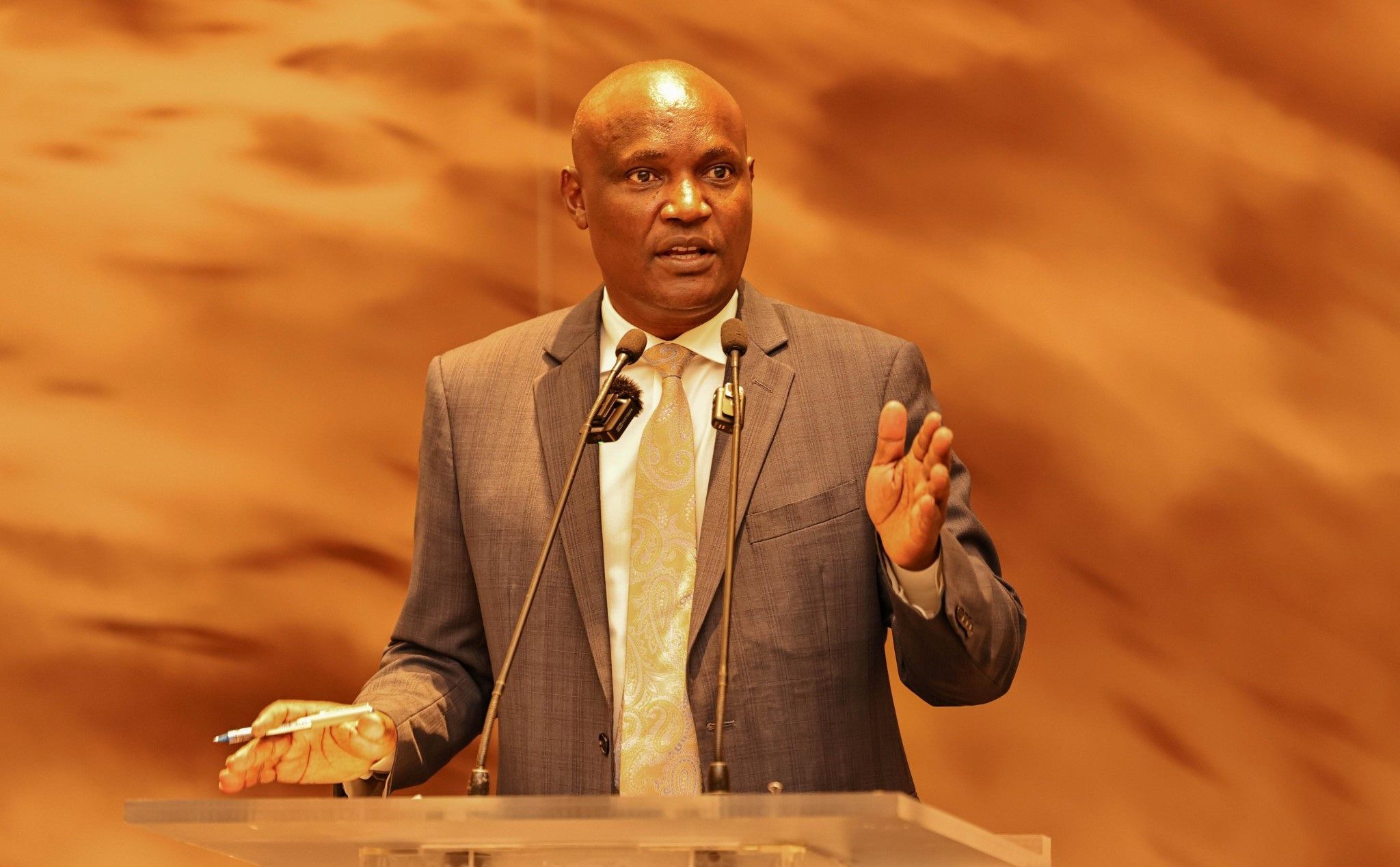
Dr. Rose Wafula, head of the National AIDS and STI Control Programme (NASCOP), discussed the limitations of the current two-test strategy in a recent KTN News interview. "Recent evidence shows that the two-test algorithm has limitations at the population level, leading to cases that are not correctly classified for appropriate intervention," she explained.
"The new three-test algorithm increases our opportunity to correctly classify individuals at the point of service within a shorter time, providing accurate results and guiding them to the correct treatment," she added.
The Kenya HIV Prevention Revolution Roadmap 2030 outlines the country's ambitious goals for HIV prevention, including a 75 per cent reduction in new HIV infections among adults by 2025, lowering mother-to-child transmission rates to less than 5 per cent, decreasing STI incidences, and achieving the micro-elimination of viral hepatitis.
It also emphasises the need for a targeted approach to HIV prevention.
Key HIV epidemic and programme coverage indicators reveal significant gaps in several counties, including Mombasa, Kisumu, Siaya, Nairobi, Kisii, Homa Bay, Migori, Busia, Kakamega, Nakuru, Kiambu, and Uasin Gishu, which require intensified efforts to curb new HIV infections. Marsabit County is also experiencing an emerging HIV epidemic that needs urgent attention.
The Ministry of Health encourages healthcare providers and the public to support ongoing surveillance efforts to maintain the integrity of testing services. Kenya ranks seventh globally in terms of its HIV epidemic and continues to deliver comprehensive care and preventive measures for the approximately 1.4 million people living with HIV.
According to the National Syndemic Diseases Control Council (NSDCC), the first HIV case in Kenya was detected in 1984. By the mid-1990s, HIV had become a major cause of illness, heavily straining the healthcare system and economy.
Other Topics To Read
In 1996, 10.5 per cent of Kenyans were living with HIV, but through extensive efforts in scaling up treatment and care, the prevalence rate nearly halved to 5.9 per cent by 2015. By 2016, 64 per cent of people living with HIV were on treatment, with 51 per cent achieving viral suppression.
Kenya's HIV epidemic, primarily driven by sexual transmission, affects all segments of the population, including children, young people, adults, women, and men. As of 2015, 660,000 children had been orphaned by AIDS. However, a disproportionate number of new infections occur among key populations.
In 2020, it was estimated that 30 per cent of new annual HIV infections in Kenya were among these groups.
Top Stories Today