WHO accelerates development of mRNA vaccines for bird flu
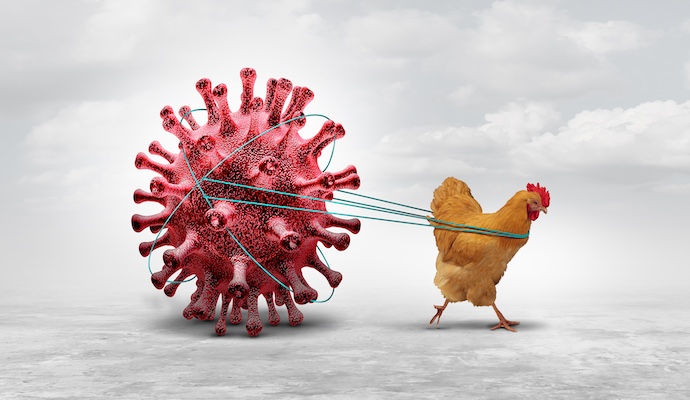
Avian influenza viruses pose a serious public health risk because they are commonly found in animals and have the potential to cause a future pandemic.
The World Health Organisation (WHO) has launched a new initiative to accelerate the development and availability of human avian influenza (H5N1) mRNA vaccine candidates for manufacturers in low- and middle-income countries.
Avian influenza, commonly known as "bird flu," primarily infects birds but can occasionally spread to humans. The most prevalent strain affecting humans is Influenza A (H5N1), which can cause severe respiratory symptoms.
More To Read
- Malaria: Drug resistance and underfunding threaten progress towards eliminating killer disease
- Sudan’s crisis deepens with communities trapped in ‘siege conditions’
- Adult obesity treatment enters new era with WHO-endorsed GLP-1 drugs
- Flu shots: how scientists around the world cooperate to choose the strains to vaccinate against each year
- Study flags stark inequities in global epilepsy care, medication
- WHO warns of measles resurgence as vaccine gaps widen
Those most at risk include individuals working with poultry, waterfowl (such as geese and ducks), and livestock.
Kenya, due to its location along migratory bird routes and proximity to high-risk areas, is particularly vulnerable to avian influenza.
The Technology Transfer Programme aims to help countries improve their ability to research, develop, and make vaccines so they are better prepared for future pandemics.
Launched initially in July 2021 by WHO and the Medicines Patent Pool (MPP) to build vaccine production skills in low- and middle-income countries, Sinergium Biotech, a partner in the programme, has developed potential H5N1 vaccines and is testing them in early studies.
Dr Tedros Adhanom Ghebreyesus, WHO Director-General, emphasised, "This initiative highlights the purpose of the mRNA Technology Transfer Programme—to promote greater research, development, and production in LMICs, ensuring that when the next pandemic arises, the world will be better prepared to respond effectively and equitably."
 WHO Director-General Tedros Adhanom Ghebreyesus speaks during a press conference at the WHO headquarters in Geneva. (AFP)
WHO Director-General Tedros Adhanom Ghebreyesus speaks during a press conference at the WHO headquarters in Geneva. (AFP)
Upon completion of preclinical data, technology, materials, and expertise will be shared with other manufacturing partners to expedite the development of H5N1 vaccine candidates and enhance pandemic preparedness efforts.
Charles Gore, Executive Director of MPP, noted, "When we established the mRNA Technology Transfer Programme with WHO, our goal was to enable LMICs to take the lead in development, foster collaboration, share resources, and disseminate knowledge. This project reflects our vision and demonstrates a strong commitment to future pandemic preparedness and response."
Dr. Jarbas Barbosa, Director of the Pan American Health Organisation, emphasised the importance of diversifying the innovation and production of health technologies across different regions.
He acknowledged the capabilities present in Latin America and the Caribbean and stressed the necessity of early planning to ensure access to and the sharing of knowledge and technologies during research and development.
Dr. Alejandro Gil, Chief Executive Officer of Sinergium, added, "Sinergium’s enhanced capabilities and readiness to apply our expertise to H5N1 will be crucial for global pandemic preparedness. We value PAHO’s support for regional manufacturers in the Americas and look forward to tackling this public health challenge with our R&D team working closely with programme partners."
Since its launch, the mRNA Technology Transfer Programme has built and validated a platform to test the effectiveness, safety, and immune response of a COVID-19 vaccine in animal models. Afrigen, the organisation that developed this platform, is now sharing the technology with other manufacturers to adapt it for other important diseases.
The progress of this programme is crucial to WHO and MPP’s goal of making mRNA vaccines more accessible and equitable worldwide.
 Lab technician at Afrigen, the Cape Town-based firm hosting the WHO co-sponsored Vaccine Technology Transfer Hub. (Photo: WHO)
Lab technician at Afrigen, the Cape Town-based firm hosting the WHO co-sponsored Vaccine Technology Transfer Hub. (Photo: WHO)Lab technician at Afrigen, the Cape Town-based firm hosting the WHO co-sponsored Vaccine Technology Transfer Hub.
Argentinian manufacturer Sinergium Biotech will take the lead on this project, using the mRNA Technology Transfer Programme created by WHO to drive forward this important work.
Avian influenza viruses pose a serious public health risk because they are commonly found in animals and have the potential to cause a future pandemic. This initiative supports current efforts under the Pandemic Influenza Preparedness Framework by enhancing the sharing of influenza viruses that could lead to pandemics and improving vaccine access for low- and middle-income countries.
According to the World Health Organisation, seasonal influenza affects around one billion people annually, with 3 to 5 million cases classified as severe.
The disease results in between 290,000 and 650,000 respiratory deaths each year. Nearly all deaths from influenza-related lower respiratory tract infections in children under 5 years old occur in developing countries.
Symptoms usually begin 1–4 days after infection and typically last about a week.
Top Stories Today