Prolonged use of painkillers linked to rising cases of gastric ulcers

WHO has identified antimicrobial resistance as a major global health concern, directly attributing 1.3 million deaths to it.
Headaches are common for many people, with some considering them a normal part of life and managing them through methods like drinking plenty of water while others rely on pain relievers. For some, headaches are mild and manageable but a daily struggle for others.
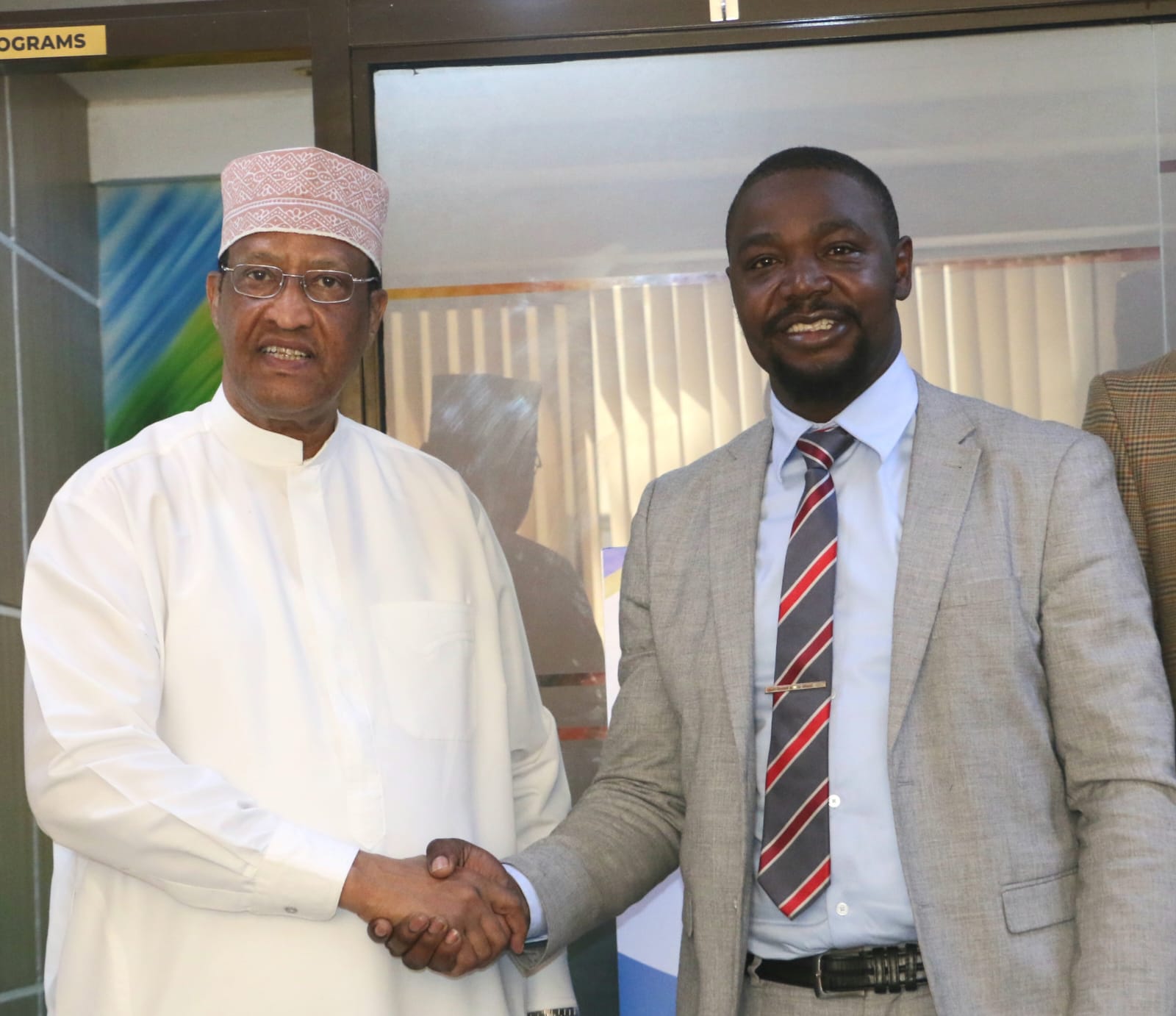
Due to the demands of his job, Alex Cyrus frequently finds himself experiencing a series of headaches and pains. To function effectively, he must find a reliable way to alleviate this constant discomfort.
More To Read
- African nations pledge to boost local manufacturing of medical products
- Kenya leads push for stronger regulation of medicines, vaccines in Africa
- Surviving the next pandemic could depend on where you live
- WHO urges countries to protect health budgets amid aid reductions
- KMPDC launches 2026 licence renewal for doctors, health facilities
- Pharmacy and Poisons Board flags falsified batch of Avastin (Bevacizumab 100 mg)
"I’ve become reliant on coffee because it helps relieve my headaches. However, when the pain becomes severe, I must resort to painkillers. I drink coffee daily, but at least once a week, I find myself needing to get painkillers from the pharmacy. Without these options, the throbbing in my head is so intense that it severely impairs my ability to function."
Alongside his frequent headaches, Cyrus also suffers from episodes of gastric ulcers, which he developed at the age of 14. He has taken to managing these ulcers on his own, dealing with the discomfort and pain as best as he can.
“I rarely go to the hospital; I reserve that option for when painkillers have proven ineffective in relieving my discomfort. Most of the time, I visit the pharmacy, where I explain my symptoms and obtain the necessary pain medication. For managing my ulcers, I concentrate on maintaining a careful diet and avoiding prolonged periods without food," Cyrus told The Eastleigh Voice.
To manage headaches and other types of pain, some people keep a stock of pain medications for daily use and become worried when their supplies dwindle. However, they often overlook the significant risks associated with long-term use of analgesics, which can lead to serious health issues.
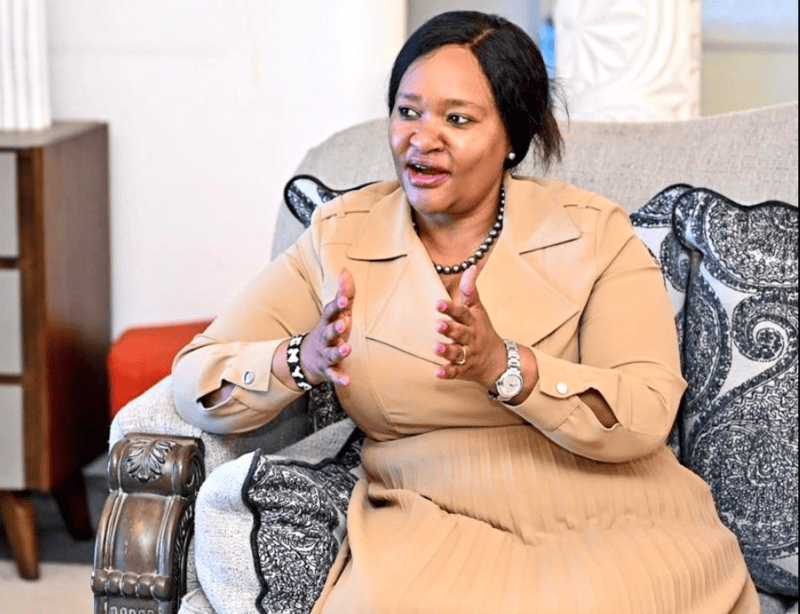
Dr Esther Mwaura, who works at a hospital in Eastleigh, said that she frequently sees patients who have become overly dependent on analgesics, with some having progressed from using recommended medications to needing much stronger painkillers.
She said sometimes patients require potent analgesics because the milder options no longer work while others opt for strong painkillers even when their pain is manageable.
“When a patient arrives, we assess and gauge the pain level to determine the appropriate treatment. As medical professionals, we often identify when the pain isn't severe enough to warrant certain options. However, some patients persist in demanding these treatments, despite our advice against them. Long-term misuse of analgesics can have serious consequences, including microbial resistance and gastric ulcers, which, if left untreated, can lead to severe complications,” said Mwaura.
 Alex Cyrus frequently finds himself experiencing a series of headaches and pains due to the nature of his work. (Photo: Eastleigh Voice)
Alex Cyrus frequently finds himself experiencing a series of headaches and pains due to the nature of his work. (Photo: Eastleigh Voice)Alex Cyrus frequently finds himself experiencing a series of headaches and pains due to the nature of his work. (Photo: Eastleigh Voice)
Microbial resistance, also known as antibiotic resistance, occurs when microorganisms such as bacteria, viruses, fungi, or parasites evolve to become resistant to the effects of medications that normally treat infections caused by these organisms. As a result, standard treatments become less effective or even ineffective, leading to persistent or more severe infections.
"We are observing a growing incidence of microbial resistance in patients, where even the most potent drugs fail to work, which is quite alarming. Additionally, we are seeing a rise in gastric ulcers. While ulcers can be caused by various factors, prolonged use of painkillers is a significant contributing factor."
Frequent use of analgesics can lead to increased use of antibiotics as a preventive or corrective measure, which in turn may worsen resistance issues. The World Health Organisation (WHO) has identified antimicrobial resistance as a major global health concern, directly attributing 1.3 million deaths to it.
The rising trend of self-medication, purchasing non-prescription drugs, and self-diagnosis is driving the increase in antimicrobial resistance (AMR), with global data reflecting a concerning upward trend.
AMR occurs when bacteria, viruses, fungi, or parasites evolve and become resistant to medications, making infections more difficult to treat and increasing the risk of disease spread, severe illness, and death.
According to the Institute for Health Metrics, Kenya reported 8,500 deaths directly attributable to AMR and 37,300 deaths associated with AMR in 2019. This places Kenya 177th in terms of age-standardised mortality rate per 100,000 population out of 204 countries.
Kenya is actively working with various institutions to combat AMR across East Africa through a comprehensive regional initiative that integrates efforts in human health, animal health, and environmental sectors.
The WHO warns that without effective measures, annual deaths due to AMR could rise to as many as 10 million by 2050. Antimicrobial medicines are crucial to modern medicine, and the rise of drug-resistant pathogens threatens the ability to treat common infections and perform life-saving procedures, including cancer chemotherapy, caesarean sections, hip replacements, and organ transplants.
Moreover, drug-resistant infections also affect animal and plant health, reduce farm productivity, and pose risks to food security. AMR places significant financial burdens on health systems and national economies by requiring more expensive and intensive care, extending hospital stays, and impacting agricultural productivity.
Top Stories Today