Govt to disburse Sh4.5 billion to settle NHIF healthcare claims

To ensure transparency in the payment process, the Ministry said a committee will be formed to oversee the disbursement.
The government is set to release Sh1.5 billion this week to address outstanding claims owed to healthcare facilities, with an additional Sh3 billion scheduled for disbursement next week.
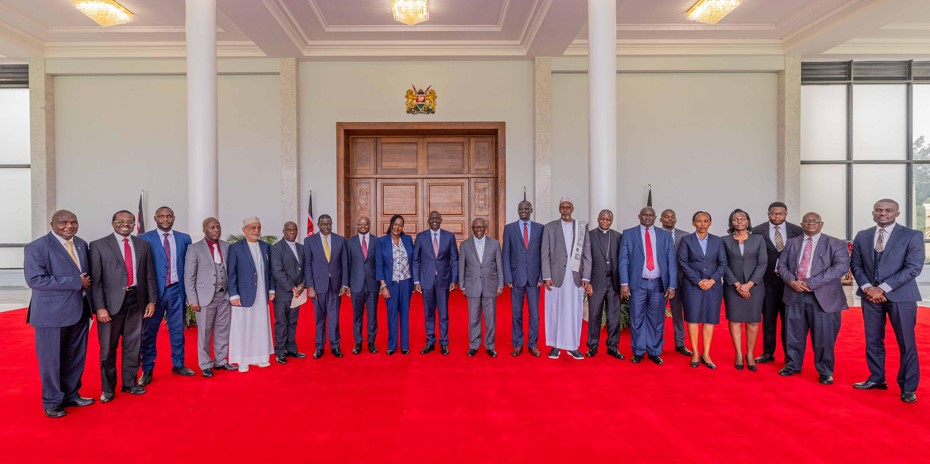
Principal Secretary for Medical Services Harry Kimtai on Tuesday confirmed that all claims owed by the National Hospital Insurance Fund (NHIF) will be fully settled.
More To Read
- KNCHR says Kenyans still locked out of healthcare despite Sh138 billion SHA boost
- MPs ditch SHA, the public health scheme they once praised, and opt for private cover
- How Trump–Ruto health deal fills the void left after USAID exit
- MPs demand SHA clears Sh10 billion in pending NHIF bills within three months
- TSC confirms shift to SHA cover for teachers from December 1
- SHA transition sparks tension as teachers cite lack of consultation, legal violations
The Ministry of Health noted that as of Monday, October 14, over Sh100 million in claims had already been recorded, allowing for real-time monitoring of the payment system.
The PS further assured that all outstanding claims would be resolved within 90 days.
“We are optimistic that we will settle all the claims,” he said.
To ensure transparency in the payment process, the Ministry said a committee will be formed to oversee the disbursement.
Kimtai also noted that NHIF liabilities have now transitioned under the Social Health Authority (SHA), which has introduced a fully digitised claims portal.
In addition to settling claims, he said the SHA is working on digitising health records and will provide tablets to healthcare workers.
“This will transform our healthcare system,” Kimtai said, emphasising the shift to e-contracting for healthcare facilities, replacing the previous manual processes.
He also encouraged healthcare facilities to set up customer service desks to assist Kenyans in registering with SHA.
Since its launch on October 1, 2024, the SHA platform has received over 940 claims valued at more than Sh12 million from healthcare providers, according to a recent survey conducted by the Rural Urban and Private Hospitals Associations.
The survey shows that the SHA portal, designed to manage claims under the new health insurance scheme, has registered submissions from over 288 healthcare providers.
Kenyatta National Hospital (KNH) submitted the highest number of claims, totalling Sh2.3 million for reimbursement within the first nine days of the new system's operation. KNH led the claims submissions with 87 claims, followed by Rapha Dialysis and Diagnostic Centre, which submitted 60 claims worth Sh682,000.
Cure and Cure Hospital recorded 37 claims totalling Sh626,000. Other facilities, including Tophill Hospital in Eldoret, PCEA Chogoria Hospital, Ladman Hospital, and Tenwek Hospital, also submitted significant claims ranging from Sh362,000 to Sh534,000.
The data reveals that inpatient claims account for the majority of costs, with 343 claims amounting to Sh7.2 million, while outpatient claims reached Sh5.2 million from 567 submissions.
The government has paid Sh1.5 million for 94 claims so far, but concerns over the system's readiness remain. The report notes that many hospitals reported issues accessing the SHA portal, resulting in delays in submitting claims.
Top Stories Today