Conflict, climate change, and poor hygiene practices fuel cholera resurgence

Cholera's resurgence extends beyond technical failures; it is deeply intertwined with broader systemic issues such as conflict, climate change, and social inequities.
The ongoing global failure to implement effective water, sanitation, and hygiene (WASH) practices has led to the continued spread of cholera.
Despite global commitments to Sustainable Development Goal 6, which seeks universal access to sustainable water and sanitation, a 2020 World Health Organisation (WHO) report revealed that 2 billion people lacked safe drinking water. Only 54% of the global population had access to safely managed sanitation services, and around 30% lacked basic handwashing facilities at home.
More To Read
In January 2023, the World Health Organisation declared the current resurgence a grade 3 emergency, reporting over 500,000 cases, particularly in Afghanistan, Haiti, and the Democratic Republic of the Congo, leading to 4,007 deaths—an alarming 71% increase from the previous year.
The declaration compounds the fact that cholera, which is easily preventable and treatable, has claimed millions of lives since the onset of the seventh pandemic in 1961, primarily driven by the El Tor biotype.
Cholera's resurgence extends beyond technical failures; it is deeply intertwined with broader systemic issues such as conflict, climate change, and social inequities. Armed conflicts disrupt or dismantle health systems, while extreme weather events and climate-related stressors compromise water safety, increasing the risk of waterborne diseases like cholera.
For instance, Haiti, once cholera-free, faced a catastrophic outbreak after UN peacekeepers inadvertently introduced the disease following the 2010 earthquake, leading to its current endemic status. Recently, Sudan has encountered a major cholera outbreak exacerbated by severe conflict and climate-related flooding, which has severely impacted health facilities and caused mass displacement, complicating disease control efforts.
Similarly, recent flooding in Nigeria has displaced many individuals, straining already limited resources and complicating responses to the country's largest cholera outbreak in decades. The Nigerian government has faced criticism from civil society for its inadequate response to recurring cholera outbreaks, emphasising the urgent need for significant investment in water and sanitation.
In Kenya, ongoing humanitarian crises, worsened by climate change and political instability in neighbouring Somalia, have increased vulnerability. Displacement into overcrowded and underresourced camps has heightened the risk of cholera transmission.
 People walk through floodwaters after heavy rainfall in Hadeja, Nigeria. Photo : Handout
People walk through floodwaters after heavy rainfall in Hadeja, Nigeria. Photo : Handout
Since 2014, Kenya has faced recurrent large-scale cholera outbreaks, reporting 10,568 cases in 2015 and 5,208 in 2019. As of October 2023, the country reported 12,120 cases, with a case fatality rate of 1.7%.
In response to these challenges, the Ministry of Health initiated the "Epuka Uchafu Nyumbani" WASH programme to improve sanitation. The Health Principal Secretary said the initiative is a vital step in Kenya's battle against public health challenges.
This initiative aims to promote disease prevention through enhanced personal hygiene, environmental cleanliness, and proper water and sanitation practices. The PS noted that with Kenya generating around 22,000 metric tonnes of waste daily—only 10 per cent of which is managed properly—and 7.3 per cent of households lacking basic sanitation facilities, the initiative focuses on empowering communities to develop sustainable, locally-driven solutions for waste management.
Muthoni highlighted the importance of community engagement, stating, "This initiative is about more than just waste management; it's about ensuring a healthier, safer future for all Kenyans by empowering communities to take charge of their environment and well-being."
However, insufficient implementation in slums and underserved communities has left these areas especially vulnerable, raising the risk of cholera and other preventable diseases. The neglect can largely be attributed to the failure to implement effective WASH practices.
Residents in the slums often feel left behind, facing dire sanitation conditions that seem insurmountable. For many, poor sanitation remains a daily reality, underscoring the urgent need for targeted interventions to improve their living conditions.
Other Topics To Read
In many countries, WASH initiatives have relied excessively on a combination of donor funding and local, non-professional solutions. An upcoming Lancet Commission on WASH will further investigate these challenges.
Kenya also launched the National Multi-Sectoral Cholera Elimination Plan in 2022, aiming for a 90% reduction in cholera deaths by 2030.
This aligns with the Global Task Force on Cholera Control plan to reduce cholera deaths by 90% from 2015 levels by 2030, a goal that seems increasingly unlikely without immediate and coordinated action.
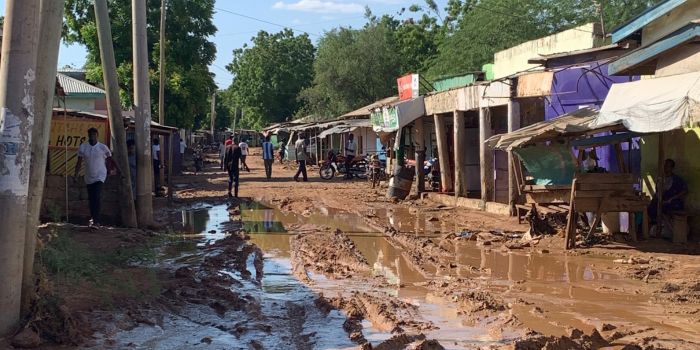 A deserted commercial street in the Winsor area of Garissa Township, as pictured on May 19, 2024, following heavy rain and flooding. (Photo: Issa Hussein/EV)
A deserted commercial street in the Winsor area of Garissa Township, as pictured on May 19, 2024, following heavy rain and flooding. (Photo: Issa Hussein/EV)
Despite the plans put in place, there have been significant shortcomings in providing cholera vaccination and treatment. Although Gavi has distributed millions of doses, production and distribution bottlenecks have led to fragile supply chains, with EuBiologics as the sole manufacturer.
A global stockpile of oral cholera vaccines for emergency use was created in 2013, starting with 2 million doses. By 2023, production had increased to 36 million doses, yet the stockpile was completely depleted earlier this year, despite efforts to maximise reserves by switching from a two-dose to a single-dose regimen for outbreak responses.
Gavi expects that the recent prequalification of the new simplified vaccine, Euvichol-S, which has similar efficacy to existing vaccines, will help alleviate shortages by 2025 due to its easier and more cost-effective production.
While technical interventions are crucial, addressing root causes—such as conflict, displacement, and extreme poverty—is vital to controlling cholera's ongoing threat.
Top Stories Today


















