Tackling antimicrobial resistance: A growing concern for Kenya, rest of the world

In Kenya in 2019, there were 8,500 deaths attributable to AMR and 37,300 deaths associated with AMR.
The misuse of antibiotics is a significant driver of antimicrobial resistance (AMR), particularly in emergency care settings, where studies estimate that 40–60% of cases involve inappropriate use.
As the world observes AMR Week, AMR threatens to undo decades of progress in combating infectious diseases.
More To Read
- WHO warns of rising antimicrobial resistance in fungal infections
- Ministry warns Kenyans on escalating antibiotic resistance
- WHO sounds alarm: Antibiotic resistance rising fast, puts millions at risk worldwide
- WHO raises alarm as antibiotic resistance threatens global health gains
- Kenya's public health at risk as falsified and substandard medicines accelerate antimicrobial resistance
- Clean hands, safe bites: Why everyday food habits matter more than you think
In Kenya in 2019, there were 8,500 deaths attributable to AMR and 37,300 deaths associated with AMR. Kenya has the 28th highest age-standardised mortality rate per 100,000 population associated with AMR across 204 countries. According to the Institute of Health Metrics and Evaluation.
Antimicrobial resistance (AMR) occurs when microorganisms like bacteria, viruses, fungi, and parasites evolve to resist the drugs that once killed them or inhibited their growth. This resistance makes infections harder to treat, leading to longer illnesses, higher healthcare costs, and increased mortality.
In Kenya, the rising threat of AMR is a critical concern. Several factors contribute to the situation:
Overuse and misuse of antibiotics
Antibiotics are often prescribed for viral infections (where they are ineffective), or people self-medicate without proper guidance. This misuse accelerates the development of resistant strains.
Access to healthcare
Inadequate access to quality healthcare, particularly in rural areas, can result in incomplete courses of antibiotics or improper treatment regimens, fostering resistance.
Agricultural use
The widespread use of antibiotics in livestock farming can contribute to the emergence of resistant bacteria, which can be transmitted to humans through consumption of contaminated food or direct contact with animals.
Lack of awareness
Public and healthcare workers may not fully understand the dangers of AMR, contributing to its persistence.
Antimicrobial Resistance (AMR) affects not only humans but also livestock and other animals. The overuse and misuse of antibiotics in veterinary medicine contribute significantly to the development of AMR in animals, which can then be transmitted to humans, exacerbating the public health threat.
A 2024 study titled "Examining Antibiotic Use in Kenya: Farmers' Knowledge and Practices in Addressing Antibiotic Resistance" revealed that around 80% of households use antibiotics for their livestock, with 58% administering them without professional help.
The majority of farmers buy antibiotics without a prescription, using them for both treatment and non-therapeutic purposes, such as promoting growth and enhancing feed in poultry. The withdrawal periods reported by farmers were often shorter than the recommended guidelines.
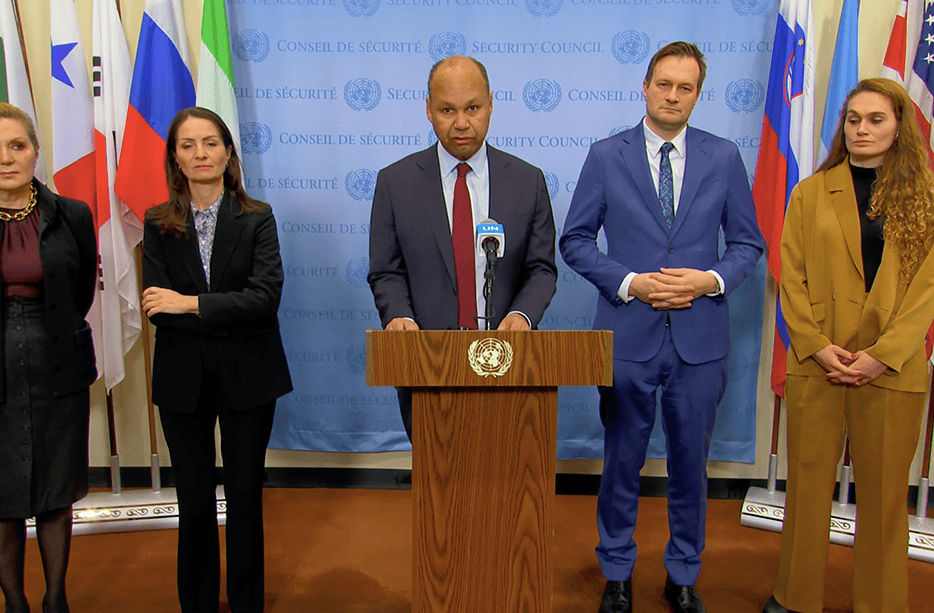
 French Ambassador to Kenya Arnaud Suquet and Kenya Red Cross Secretary-GeneralAhmed Idris during the signing of the partnership agreement to combat antimicrobial resistance on May 10, 2024. (Photo: Kenya Red Cross)
French Ambassador to Kenya Arnaud Suquet and Kenya Red Cross Secretary-GeneralAhmed Idris during the signing of the partnership agreement to combat antimicrobial resistance on May 10, 2024. (Photo: Kenya Red Cross)
Although many farmers acknowledged risky antibiotic practices, 76% were aware of bacterial AMR. Respondents correctly answered 55–89% of 21 knowledge statements on AMR and safe antibiotic use, indicating good awareness, though certain gaps remain. The number of livestock owned was the main factor influencing farmers' knowledge of AMR and safe antibiotic use.
Impact in Kenya
Increased Mortality: AMR leads to longer and more complicated infections, raising death rates from conditions like pneumonia, tuberculosis, and sepsis, which are common in Kenya.
Economic Strain: The rising costs of treating resistant infections place a significant burden on both individuals and the healthcare system. More expensive drugs, longer hospital stays, and the need for more advanced care add to the financial strain.
Public Health Challenge: As resistance spreads, diseases that were previously manageable could become harder to treat, making it difficult for Kenya to achieve health goals such as reducing child mortality or controlling infectious diseases.
In 2022, Kenya developed a National Action Plan on Antimicrobial Resistance (AMR), identifying key gaps and highlighting findings to accelerate human health sector progress. The plan targets all stakeholders in implementing actions to address AMR in the country. The Kenya Red Cross has teamed up with the French Embassy in Nairobi to tackle the growing threat of AMR.
The project involves partnerships with the Kenya Red Cross, the International Livestock Research Institute (ILRI), and the Kenya Medical Research Institute (KEMRI). According to the World Health Organization (WHO), AMR is one of the most urgent global public health and development challenges. In 2019, AMR directly caused an estimated 1.27 million deaths and contributed to a total of 4.95 million deaths worldwide.
A recent report by The Lancet forecasts that over 39 million people globally will die from antibiotic-resistant infections between now and 2050. The report also predicts that by 2050, approximately two million deaths annually could be attributed to drug-resistant infections.
As the world observes AMR Awareness Week, The World Health Organisation (WHO) recommends six steps we can all take year-round to help prevent antimicrobial resistance (AMR):
Understand the facts: Antibiotics, or 'Thnam sas,' are effective only against bacterial infections, not viral ones like avian influenza, seasonal flu, the common cold, or COVID-19. Symptoms such as general pain, sore throats, fever, and runny nose are often not treatable with antibiotics.
Follow professional advice: Only take antibiotics, antifungals, antivirals, antimalarials, antiparasitics, and anthelmintics when prescribed by a certified healthcare professional.
Avoid using leftover antibiotics or sharing them: Never use antibiotics that were prescribed for a previous illness, and never share them with others.
Complete your prescribed medication: Finish your entire course of treatment as advised by your healthcare provider, even if you start feeling better before finishing.
Manage common viruses at home: If you have symptoms like cough, sore throat, fever, headache, or fatigue, stay home and treat the symptoms. If you have a bacterial infection, consult a healthcare provider.
Prevent infections: Get vaccinated, wash your hands regularly with soap and water (especially before eating and after using the toilet), and practice safer sex to reduce the risk of infections.
Top Stories Today