WHO approves injectable lenacapavir in major shift on HIV prevention
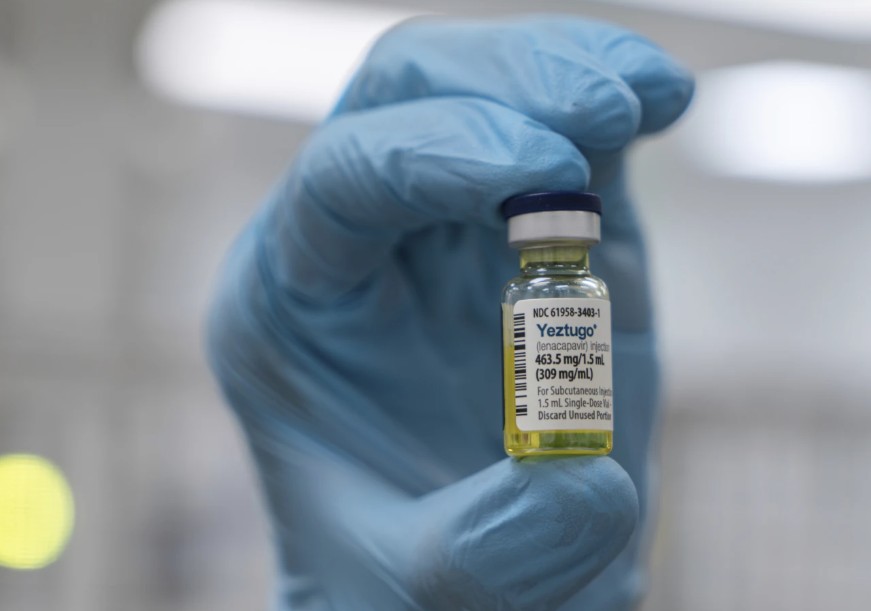
Lenacapavir is the first long-acting injectable HIV prevention drug that requires administration only twice a year. It offers a highly effective and convenient alternative to daily pills.
The World Health Organisation (WHO) has endorsed injectable lenacapavir (Leparavine) as a new option for HIV prevention, recommending its use twice a year.
The announcement was made at the 13th International AIDS Society Conference (IAS 2025), held in Kigali, Rwanda. This marks a significant step forward in HIV prevention efforts, particularly for communities that struggle with adherence to daily oral medications.
More To Read
- Vaccine hesitancy: Inside Kenya’s push against measles, rubella and typhoid
- UNAIDS warns HIV crisis could claim 4 million lives by 2029 without urgent global funding
- FDA approves groundbreaking twice-yearly HIV prevention shot
- MoH flags surge in youth HIV infections, calls for stronger prevention strategies
- Kenya’s war on HIV, TB and malaria faces setback as funding drops sharply
- Wajir launches campaign against HIV, teen pregnancies, GBV as new infections emerge in ASAL counties
Lenacapavir is the first long-acting injectable HIV prevention drug that requires administration only twice a year. It offers a highly effective and convenient alternative to daily pills, making it especially valuable for individuals who face stigma, difficulties with daily adherence, or limited access to consistent healthcare.
Clinical trials have demonstrated lenacapavir’s remarkable effectiveness. Among more than 2,000 participants, only two cases of HIV were recorded. In trials involving women and adolescent girls in Africa—a population often underserved by current HIV prevention methods—lenacapavir provided complete protection.
WHO emphasised that despite the current limited availability of lenacapavir outside of clinical trials, countries should begin integrating it into national HIV prevention programs immediately. The organisation also called for careful monitoring of uptake, adherence, and overall impact during the rollout phase.
Dr Tedros Adhanom Ghebreyesus, WHO Director-General, described lenacapavir as the most promising advance in HIV prevention since antiretroviral therapy began, saying, “While an HIV vaccine remains out of reach, lenacapavir is the next best thing. With near-total protection shown in clinical trials, this injectable could be a game-changer for millions.”
To help remove one of the major barriers to HIV prevention, WHO is also promoting a simplified HIV testing approach based on rapid diagnostic tests. This strategy eliminates the need for complex laboratory infrastructure, allowing long-acting PrEP options like lenacapavir and cabotegravir to be delivered through more accessible, community-based platforms, including pharmacies, health clinics, and telehealth services.
WHO’s new guidance does not stop at prevention. The organisation has also released updated recommendations for HIV treatment and service delivery. Among these is the support for the use of long-acting injectable cabotegravir and rilpivirine for individuals who are stable on daily oral antiretroviral therapy.
WHO further encourages the integration of HIV care with services for noncommunicable diseases such as hypertension, diabetes, and mental health, recognising the importance of holistic and person-centred healthcare.
For individuals living with HIV who contract mpox, WHO now recommends the rapid initiation of antiretroviral therapy and HIV testing for anyone with suspected or confirmed mpox infection. The updated guidance also includes expanded screening for asymptomatic sexually transmitted infections, particularly within high-risk populations.
Recognising the increasing financial strain on health systems, WHO has also issued operational guidance to help countries safeguard essential HIV services. This includes frameworks for assessing risks, prioritising services, and adapting systems to maintain progress and protect health outcomes even in the face of shrinking budgets.
Dr Meg Doherty, Director of WHO’s Global HIV, Hepatitis and STI Programmes, highlighted the urgency of turning these recommendations into action. “We have the tools and the knowledge to end AIDS as a public health problem,” she said. “What’s needed now is bold action—grounded in equity and powered by communities.”
By the end of 2024, an estimated 40.8 million people were living with HIV globally, with 65 per cent of them residing in the African region. Around 630,000 people died from HIV-related causes during that year, while 1.3 million became newly infected, including 120,000 children. Access to treatment continues to expand, with 31.6 million people receiving antiretroviral therapy in 2024, up from 30.3 million the previous year.
Despite its promise, lenacapavir remains out of reach for most people in low-income countries due to its high cost.
Leparavine is currently priced at levels similar to those in developed countries, making it largely unaffordable for most Kenyans. While in the United States, Europe, and Canada, the cost ranges between $28,000 and $43,000 per year—equivalent to roughly 4 to 6.5 million Kenyan shillings—the price in Kenya is expected to be similar if no special subsidies or generic options become available.
Encouragingly, 2024 brought a breakthrough. Gilead Sciences, the manufacturer of lenacapavir, granted royalty-free licenses to six generic drug companies: Dr. Reddy's Laboratories, Emcure Pharmaceuticals, Hetero Labs, Viatris' Mylan unit, Eva Pharma, and Ferozsons Laboratories. These licenses cover 120 low- and lower-middle-income countries, including Kenya, and will allow the production of generic versions at a fraction of the cost.
When these generics become available, the annual cost of lenacapavir could drop to as little as $40—a drastic reduction that would transform access across the Global South. Meanwhile, Gilead has committed to supplying the branded version of the drug in 18 countries, including Kenya, Botswana, and Ethiopia, until local manufacturers are ready to meet demand. These countries together account for about 70 per cent of global HIV cases.
To support this effort, the Global Fund is collaborating with private-sector donors, including the Children’s Investment Fund Foundation (CIFF), to fund the introduction and scale-up of lenacapavir in priority countries. This approach is designed to reduce financial barriers and speed up access to the drug for those most in need.
In 2024 alone, an estimated 1.3 million people acquired HIV. The highest infection rates remain among vulnerable and key populations, including sex workers, men who have sex with men, transgender individuals, people who inject drugs, people in prisons, and adolescents. By endorsing lenacapavir, WHO aims to expand the range of available prevention tools and reach populations that existing strategies have failed to adequately serve.
Kenya has about 1.38 million people living with HIV, including 1.3 million adults and approximately 68,000 children. The national HIV prevalence among adults aged 15 to 49 is around 3.3 per cent, with women more affected at 4.5 per cent, compared to 2.2 per cent for men.
In 2023, Kenya recorded approximately 16,752 new HIV infections and 20,480 AIDS-related deaths, including 2,607 children. While these numbers remain high, they reflect steady progress — the country has reduced HIV infections and AIDS-related deaths by over 65 per cent since 2013.
Globally, an estimated 39 million people were living with HIV in 2023. That year saw around 1.3 million new infections and approximately 630,000 AIDS-related deaths. Sub-Saharan Africa remains the most affected region, accounting for nearly two-thirds of all global HIV cases.
Top Stories Today