Stakeholders decry gaps in cancer care under Social Health Insurance

Despite the SHA Act’s promise to guarantee affordable healthcare for all, especially those grappling with chronic and critical illnesses like cancer, the coalition jointly argues that many patients continue to face severe obstacles in accessing quality treatment.
A coalition of health and economic experts, patient advocates, and civil society groups convened on Friday in Nairobi.
This was in a joint session hosted by the National Taxpayers Association (NTA), Kenya National Cancer Network (KENCO) to scrutinise the current state of Kenya’s healthcare system.
More To Read
- Genetic tests for cancer can give uncertain results: new science is making the picture clearer to guide treatment
- Breast cancer: New study finds genetic risk in African women
- Silent crisis of self-medication and gaps in SHA services for patients with chronic illnesses
- Study shows physical exercise can greatly reduce cancer recurrence
- PS Oluga warns stigma denying thousands of PWDs vital health services
- Ruto orders action against public hospitals charging outpatient fees
Their focus: the glaring shortcomings of the Chronic and Critical Illness Fund (ECCIF) under the Social Health Insurance Act (SHA) and its impact on cancer patients.
Despite the SHA Act’s promise to guarantee affordable healthcare for all, especially those grappling with chronic and critical illnesses like cancer, the coalition jointly argues that many patients continue to face severe obstacles in accessing quality treatment.
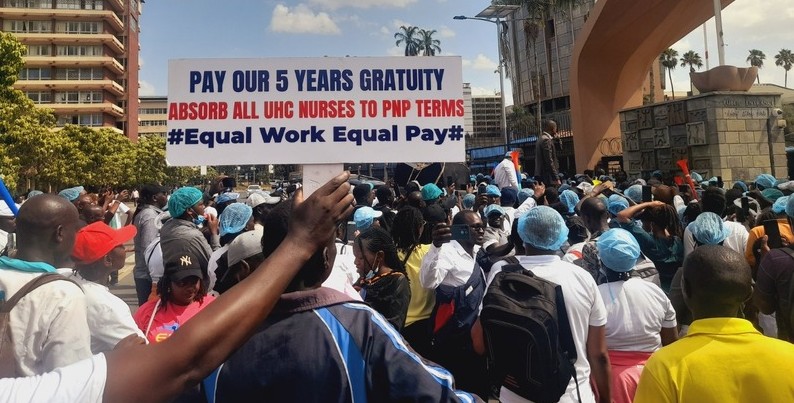
Testimonies from patients revealed frequent shortages of essential cancer drugs and palliative care medicines in public hospitals accredited by the SHA, forcing them into costly out-of-pocket expenditures, treatment delays, or even abandonment of therapy altogether.
Another key issue raised during the briefing was the inadequacy of the current oncology benefit package, which allocates Sh550,000 for cancer treatment, comprising Sh150,000 for emergency and Sh400,000 for treatment.
“This sum is way too little. On my occasions, a cancer patient could be left with less than Sh100,000 of the total Sh550,000 allocation, before starting the real treatment,” said one of the cancer survivors who spoke on anonymity.
She explained that this is because the health cover falls short in several areas, particularly in covering the full cost of cancer treatment, including the diagnostic stage, which often requires substantial financial outlay.
Moreover, confusion persists among patients and healthcare providers about eligibility criteria and access procedures for the ECCIF, compounding treatment challenges.
Critics during the session also highlighted the absence of official government documentation to formalise promised increases in Social Health Insurance Fund (SHIF) benefits.
This lack of clarity and transparency, they said, undermines consistency in applying the oncology benefits package, resulting in systemic delays and errors at accredited healthcare facilities.
The briefing also revealed that these systemic failures are not limited to service delivery but extend to broader financial inadequacies in the country's health budget.
“The financing for the cancer care continuum is grossly underfunded, with cancer being the third leading cause of death in Kenya,” NTA noted in the session's communique.
In FY 2023/24, total estimated expenditure on Non-Communicable Diseases (NCDs) prevention and control was Sh2.25 billion.
However, this amount dramatically dropped to Sh749.3 million in FY 2024/25 to rise again to Sh1.2 billion in FY 2025/26.
“This erratic funding pattern undermines long-term planning and service delivery. Spending on NCD prevention and control is inconsistent and poorly aligned with the increasing burden of disease,” said NTA CEO Patrick Nyangweso.
The stakeholders further critiqued the government's commitment to its own strategic plans, particularly the National Cancer Control Strategy 2023–2027, which requires Sh49.2 billion for full implementation.
So far, they note that less than 10 per cent of this amount has been consistently allocated, with significant gaps in screening, treatment and infrastructure development.
The Abuja declaration in 2001 requires that governments in Africa allocate at least 15 per cent of annual budget allocation to the health sector.
“Our current allocation for health stands at about three per cent. Unless this funding is scaled up and sustained, the strategy risks remaining a paper promise.”
Top Stories Today