Mtwapa HIV clinic for pregnant women ensuring babies are born disease-free

One main problem is the reluctance of some mothers to disclose their HIV status to their partners.
Women sit outside on wooden benches at a clinic in Mtwapa, Kilifi County, their faces showing a mix of anticipation and anxiety, waiting for their turn. Some are pregnant while others are holding their infants. All are here to seek services that promise a healthier future for their children.
This is where the journey begins for many HIV-positive pregnant women. Here, they get the compassionate and unwavering support of mentor mothers.
More To Read
- Out-of-pocket medicine costs surge amid drug shortages in Kenya
- UNAIDS hails Kenya–US health framework as major boost for HIV response
- Kenya's HIV statistics (2024)
- German researchers find highly effective HIV antibody
- High Court upholds ruling against KDF for HIV discrimination in recruitment
- Tanzanian woman's immune response yields antibody capable of halting most HIV variants
Mentor mothers are women living with HIV and working at the prevention of mother-to-child transmission (PMTCT) clinics to support pregnant mothers and ensure unborn babies are not infected.
The clinic, a lifeline for many women, is a sanctuary of hope and resilience.
Francisca Adhiambo is one such mentor mother. Her day starts early as she prepares for the health talk, a daily ritual that sets the tone for the day.
“Health talk is key,” she says as she addresses the group of expectant mothers.
She stresses the importance of raising an HIV-negative child and living a fulfilling life despite having an HIV-AIDS diagnosis.
“We introduce many things during the health talk. This is where we get to know our clients and start providing crucial information,” she explains.
After the health talk, Adhiambo begins screening the women.
“If a pregnant woman is found to be HIV-positive, we enrol her into our programme immediately,” she says.
The goal is to ensure that every HIV-positive mother can give birth to a healthy baby.
Counselling services
One of the most critical aspects of Adhiambo’s work is counselling. She explains to the mothers the importance of starting antiretroviral therapy as soon as possible. The mothers are supported all the until delivery to ensure they give birth to HIV-free babies.
Adhiambo says the support extends beyond the clinic walls, and if a client misses an appointment, she goes looking for her, ensuring no one is left behind.
The results of this dedication are evident.
“In 2020, we had seven babies born with HIV, but since then, the number has significantly dropped,” Adhiambo says with pride.
She says organisations like Stawisha, Kemri, and USAID have played a significant role, in providing free medication and education on living positively with HIV.
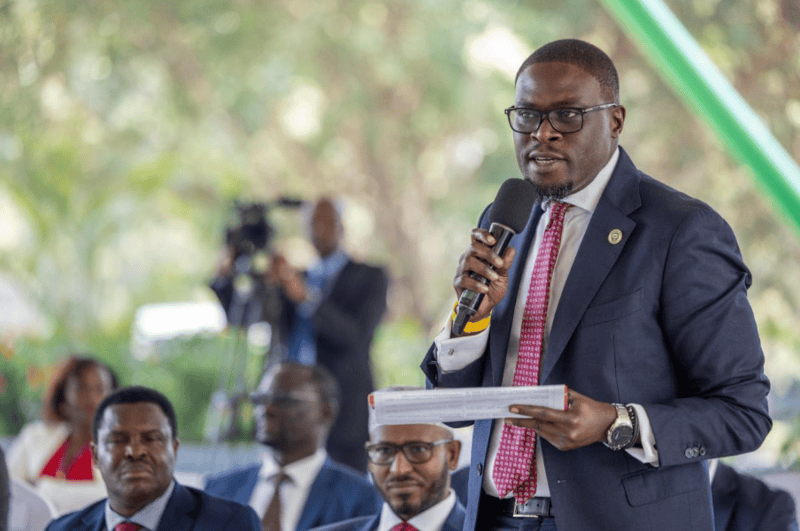
 Mtwapa Sub-County Hospital Medical Superintendent Dr Samiya Mabruk. (Photo: Farhiya Hussein)
Mtwapa Sub-County Hospital Medical Superintendent Dr Samiya Mabruk. (Photo: Farhiya Hussein)
Adhiambo says it is not always easy for them as amidst successes, they also face some challenges.
One main problem is the reluctance of some mothers to disclose their HIV status to their partners.
“We cannot force the client to disclose it, but we teach them the importance of doing it,” Adhiambo says.
Another challenge they encounter is the logistical hurdles of tracing clients who move frequently or live in distant areas.
“Sometimes, a client will say she lives in Mtwapa, but when we go there, she’s not around,” she says.
Helen Tunje, a nursing officer at Mtwapa Sub-County Hospital, recounts similar experiences.
In 2020, the hospital saw seven babies born with HIV, prompting a collaborative intervention with partners like Stawisha. The efforts have drastically reduced the number of infected babies.
“In 2021, there was only one case, and in 2022, none,” Tunje says.
Continuous monitoring, health education, and support for these mothers are crucial components of their strategy. Tunje says they monitor their patients’ viral load, provide nutrition advice, and treat any non-communicable diseases.
Tunje shares her reflections on the progress and challenges in maternal and child health services for HIV-positive mothers.
"We manage between 190 and 230 mothers, monitoring their viral loads, and educating them on nutrition and health. We feel happy when they do well, and they appreciate our support,” she says.
She says previously, they had no cohesive approach as they just handed out drugs without addressing underlying issues.
“Through the Stawisha programme, we have mentor mothers, frequent supervisions, and team meetings to tackle challenges. Despite our efforts, challenges persist. Mothers still default on appointments, citing travel upcountry. We follow up using mentor mothers and community health workers. The workload is heavy, and sometimes we can't perform necessary tests due to staff shortages and inadequate facilities,” Tunje says.
More resources
She recommends more support in staffing and resources to ensure smooth operations.
“I am proud when mothers leave our facility happy and satisfied with our services. I am committed to my nursing duties and continually educate myself and my colleagues to provide the best care possible. Each negative test result for a child feels like an achievement, reminding me why this work is so important."
The broader impact of these efforts is highlighted by Dr Samiya Mabruk, the medical superintendent at Mtwapa Sub-County Hospital.
According to her, PMTCT services are meticulously organised to focus fully on the clients, thanks to support from USAID.
“Since I started working here in 2019, we have seen significant improvements in access and the quality of services,” she states.
Despite the progress, challenges like self-conversion and staffing shortages persist.
“One of the challenges we have always faced is that despite receiving support in terms of staffing, our numbers continue to grow due to increased access,” she says.
Another issue she says is self-conversion.
“Although our facility handles clients from antenatal care to delivery, we haven't encountered any clients who have self-converted. Instead, we receive clients from private facilities who come to our facility for delivery. While our facility has bridged some gaps through the training we've received, there remains a gap in the private facilities that need to be addressed,” Samiya says.
She says there is a need to sensitise and train healthcare workers in private facilities and support them.
“I want to extend our generosity and offer support because, at the end of the day, we are all one community serving Kilifi. We all work for the mwananchi who seeks services, whether in a public or private facility. It would be a great milestone to reach the private sector and train them in capacity building to ensure they offer the same level of services as we do,” she says.
The impact of the mentor mothers extends beyond the clinic. They are embedded into the community, ensuring that no woman feels isolated or unsupported. They provide daily injections, follow-up visits, and home visits to ensure treatment adherence.
Adhiambo says if a client does not show up for their appointments, she goes looking for her, noting that this relentless pursuit ensures every mother receives the care she needs.
The results speak for themselves. Kilifi County has seen a decrease in HIV prevalence from 4 per cent in 2021 to 2.5 per cent in 2023.
the PMTCT programme has seen a significant proportion of pregnant women receiving ARV drugs, reducing the risk of transmission. The collective efforts of mentor mothers, healthcare professionals, and supportive organisations have led to this remarkable achievement.
For Adhiambo and her colleagues, the ultimate reward is seeing a healthy, HIV-negative baby being born to an HIV-positive mother.
“The dedication and compassion of mentor mothers are crucial in the fight against HIV, ensuring that more children are born free of the virus and that their mothers can live healthier, more hopeful lives,” she says.
Top Stories Today