Explainer: How Kenyans are struggling for healthcare despite UHC promise

In Kenya, the Social Health Insurance Fund (SHIF) is a key component of the government's strategy to achieve UHC) aiming to provide affordable and accessible healthcare for all citizens, including those in the informal sector and vulnerable groups.
Universal Health Coverage (UHC) was introduced globally and in Kenya to ensure that everyone, regardless of their income or location, can access quality healthcare without financial strain. It offers essential services such as doctor visits, medications, preventive care, and promotes a more inclusive society.
At the core of UHC are four key principles: access to healthcare, ensuring people receive medical attention without barriers; quality services, guaranteeing effective and safe care; financial protection, preventing medical expenses from causing poverty; and equity, ensuring fair healthcare access for all, especially vulnerable groups.
More To Read
- From free to unaffordable: Why more Kenyan women are giving birth at home again
- Counties undermining UHC by redirecting reimbursements, Health Committee says
- Report lays bare Kenya’s failing healthcare system
- SHA accused of ignoring law in hiring as NHIF workers left out
- Cancer patients stage protest outside SHA headquarters, demand better medical coverage
- Growing health crisis among Kenya’s elderly: Costs, care and insurance coverage
However, significant challenges remain, with the equity gap in healthcare access continuing to widen. Many Kenyans now struggle more than ever to receive medical care, facing a system that has failed to fully deliver on its promises.
Out-of-pocket expenses have surged, placing a heavy financial burden on households, while shortages of essential medications further exacerbate the crisis, leaving vulnerable populations without the care they need.
UHC in Kenya was first introduced as a pilot programme in 2018, targeting select counties to assess its feasibility and effectiveness. Following its initial implementation, the programme was expanded nationwide in 2022, reaching all 47 counties to ensure broader healthcare access.
In 2023, major legislative reforms were introduced to strengthen healthcare financing, streamline service delivery, and enhance the sustainability of UHC.
SHIF coverage
In Kenya, the Social Health Insurance Fund (SHIF) is a key component of the government's strategy to achieve UHC) aiming to provide affordable and accessible healthcare for all citizens, including those in the informal sector and vulnerable groups.
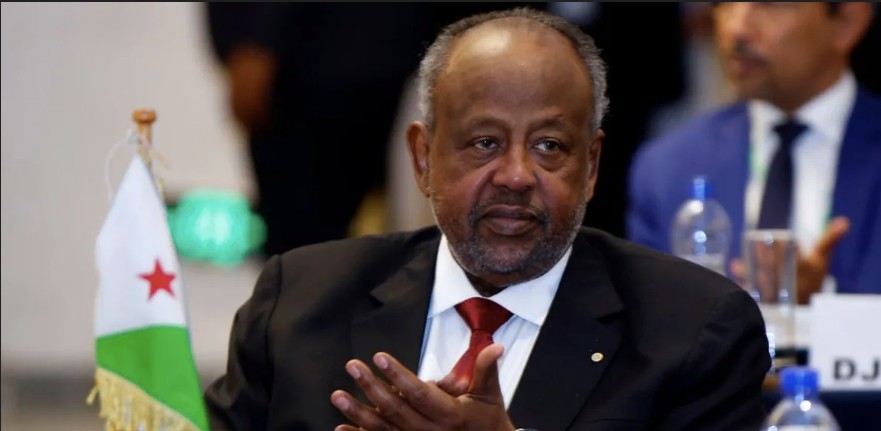
 Collins Omulo laments a lack of knowledge and awareness about UHC. (Charity Kilei)
Collins Omulo laments a lack of knowledge and awareness about UHC. (Charity Kilei)
Collins Mulo struggles to grasp the concept of UHC. He does not fully understand what it entails or how it benefits him. All he knows is that the National Health Insurance Fund (NHIF), which he relied on, was replaced by the SHIF —a system that, in his view, is not working.
"Now I know for sure that if I go to a public facility like a dispensary, I will not find medicine. When I have money, I buy my own or look for cheaper alternatives, even traditional medicine—after all, our ancestors used them."
Mulo, like many ordinary Kenyans, feels left in the dark. Information about the new health insurance system is not readily available at the grassroots level. He only hears about these changes but does not understand what they mean for him. "With NHIF, I knew it helped because I used it. But this new one—I am not even sure if I want it."
Joseph Kimani is no stranger to these struggles, yet he remains uncertain about what UHC means for him. All he knows is that healthcare has become increasingly difficult to access. The rising costs have placed a heavy burden on him, often forcing him to travel to counties such as Kiambu, where indigent patients receive financial assistance, just to find affordable care. For him, falling sick is not just about health; it is a financial crisis.
He is particularly concerned about the changes in maternal care. "I heard that women can no longer give birth for free in public hospitals unless they have paid their SHIF premiums. Before, I could take my wife to the hospital without paying anything—it was much easier."
For families like Joseph’s, the reality of Kenya’s healthcare system is not just about policies and reforms; it is a daily battle for survival.
Despite global progress towards UHC, half of the world's population still lacks access to essential healthcare services. According to the World Health Organisation (WHO), nearly 12%—around 800 million people—spend more than 10% of their household income on medical expenses, pushing nearly 100 million individuals into extreme poverty each year due to out-of-pocket healthcare costs.
The situation is even more dire in Africa. Although the continent is home to 11% of the global population, it bears 24% of the world's disease burden while accounting for less than 1% of global health expenditure.
Chronic underfunding, a shortage of healthcare professionals, and persistent health financing challenges have left most African nations struggling to provide adequate medical care. Low per capita income, limited domestic revenue generation, and systemic inefficiencies further hinder governments from effectively addressing the region’s healthcare needs.
With dwindling foreign aid, achieving equity in healthcare seems like an increasingly distant dream for countries such as Kenya, where economic hardships have made affordable medical care more urgent than ever. While UHC is designed to cushion citizens by ensuring fair and accessible healthcare, the SHIF presents contradictions—promising equitable care while imposing higher premiums.
The mandatory 2.75% contribution has placed a heavy financial strain on salaried Kenyans, while many in the informal sector have chosen not to enrol, further widening the healthcare access gap. As of last month, only about 3.3 million Kenyans had completed the scientific means testing required to determine eligibility, leaving over 15 million registered SHIF members unable to access care unless they pay out of pocket.
Many have opted out due to confusion, scepticism, or financial constraints. Leaders have increasingly questioned the sustainability of a premium-based system for funding UHC, arguing that it undermines the very principle of universal access.
Busia Senator Okiya Omtatah, seeking clarity on the scheme, confronted Health CS Deborah Barasa in the Senate over the SHIF concept, universal healthcare, and premium payments.
“Conceptually speaking, how do you reconcile the concept of universal healthcare and the practice of paying premiums? Paying premiums means that you have the capacity; universal means nobody is left behind, so how does it become universal healthcare when people have to pay a premium to access the service (SHIF)?”
While the Ministry of Health insists it is addressing the issue, the vision of UHC risks slipping away. The rising financial burden, coupled with limited benefits, undermines the very principle of accessible and quality healthcare, ultimately leaving many behind.
The reality on the ground tells a different story. Public hospitals continue to grapple with chronic medication shortages, a failing healthcare system, and an overreliance on out-of-pocket payments.
The cycle of doctors’ strikes, unresolved Collective Bargaining Agreements (CBAs), and repeated broken promises has further deepened the crisis. As financial burdens mount and benefits remain limited, the core promise of UHC—affordable, accessible, and quality healthcare for all—is slipping further out of reach, leaving millions stranded without proper medical care.
Top Stories Today