Postpartum haemorrhage: How Kenya’s Roaming Blood Bank initiative is saving mothers' lives

Postpartum haemorrhage remains one of the deadliest complications of childbirth, claiming the lives of tens of thousands of women every year. Globally, the World Health Organisation estimates that around 70,000 women die annually due to PPH, accounting for more than 20 per cent of all maternal deaths.
Lack of blood remains one of the most urgent and persistent threats in the management of postpartum haemorrhage (PPH) in Kenya, an emergency that continues to claim the lives of women in labour daily.
Four out of every ten women who bleed to death do so simply because blood is not available when they need it most.
More To Read
- Young people must lead HIV fight, says PS Ouma Oluga
- Africa’s hidden stillbirth crisis: New report exposes major policy and data gaps
- Review meeting highlights barriers to immunisation, maternal health in Turkana
- Kenya’s maternal mortality ‘a crisis that cannot be ignored’, MP Nyikal warns
- Kenya steps up border checks as Ethiopia confirms outbreak of Marburg Virus Disease
- Governors sound alarm as 934 newborns die amid funding row in health sector
For decades, the country has collected only about 60 per cent of its annual blood requirement, leaving thousands of mothers at risk. But this year, a bold innovation, the Roaming Blood Bank, a community-driven model, is transforming how blood donation drives are conducted, and more importantly, how blood reaches women in crisis.
Kenya’s blood collection rate surged for the first time to 75 per cent of the national target with a collection of about 875 units of blood, a significant milestone credited partly to this new outreach strategy, which brings donation campaigns directly to communities.
Postpartum haemorrhage is one of the most feared complications of childbirth, a sudden, heavy loss of blood that can turn a joyous moment into a medical emergency within minutes. It occurs when a woman bleeds excessively after delivery, usually more than 500 millilitres after a normal birth or over a litre after a Caesarean section. In many cases, the bleeding is so severe and so rapid that a mother can slip into shock before help arrives.
When this happens, blood becomes the most critical resource for her survival. As her body loses blood, her organs are starved of oxygen, her blood pressure drops dangerously, and she grows weak, dizzy, or unresponsive. A transfusion is often the only option, and without enough blood, even the best medical care cannot save her.
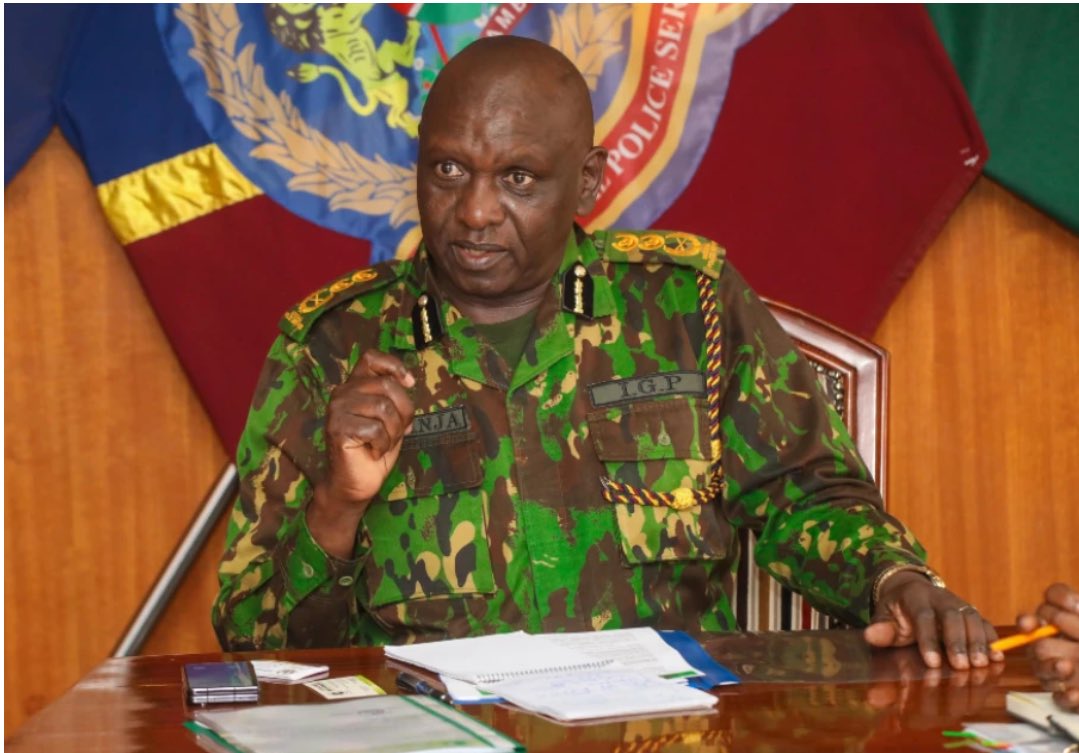
 Prof Moses Obimbo, Project Lead at End PPH Initiative, and also the Secretary to KOGS. (Charity Kilei)
Prof Moses Obimbo, Project Lead at End PPH Initiative, and also the Secretary to KOGS. (Charity Kilei)
PPH remains the leading driver of blood demand in the country. The Roaming Blood Bank initiative, officially the Rural Outreach Mobilisation Initiative for Network Growth, is championed by Professor Julius Ogeng'o of the University of Nairobi, co-lead at End PPH Initiative, a project under PPH Foundation, who has become one of its strongest advocates, working with other stakeholders like the Kenya Red Cross.
According to Prof. Ogeng'o, the model targets people across various age groups who are medically fit to donate. Volunteers not only give blood but also register their details, including blood groups and contact information. This creates a dynamic database of repeat donors who can be mobilised instantly whenever a mother, accident victim, or trauma patient requires an emergency transfusion.
“The philosophy is simple. You go to where the people are. You engage them, you build trust, and you create a network,” he explains.
Unlike the traditional model, which waits for donors to visit health facilities, the roaming teams move into estates, markets, learning institutions, worship centres, and rural communities, reminding people that donating blood is an act of humanity and a lifeline for mothers nationwide.
The pilot project was launched in September, beginning at Pumwani Maternity Hospital. In just five days, the team collected 130 units of blood.
Encouraged but determined to do more, they extended their outreach into the CBD and neighbouring areas. In just 11 days, they collected 875 units of safe blood ready for use, far above the usual 600 units.
“We are confident that we can reach all 47 counties, particularly the rural and marginalised regions, to help safeguard the lives of our mothers and sisters,” said Prof. Ogeng'o
Alongside improved blood collection efforts, Kenya is accelerating clinical interventions for PPH. Professor Moses Obimbo, Project Lead at End PPH Initiative, says their flagship awareness campaign has reached more than 15,000 people across Kenya, 10,000 of them in Nairobi alone. Through public events, including the Run for Her campaign, communities are being educated, myths are being debunked, and people are learning why PPH kills so quickly.
“Out of every ten women who die from childbirth bleeding, many die because there is no blood for transfusion,” Prof. Obimbo says. “That is why we conceived the Roaming Blood Bank to go to the people instead of waiting for them.”
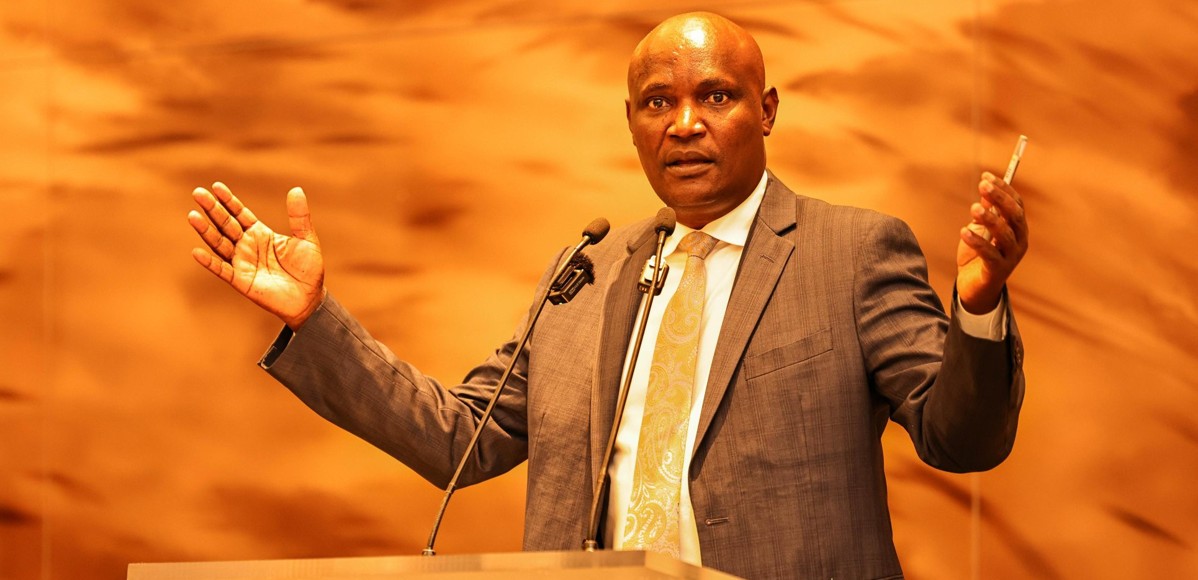
 Prof Julius Ogeng'o, a co-lead at End PPH Initiative, a project under PPH Foundation. (Charity Kilei)
Prof Julius Ogeng'o, a co-lead at End PPH Initiative, a project under PPH Foundation. (Charity Kilei)
This year, Kenya joined global partners and the WHO in launching new consolidated PPH guidelines, the first time all recommendations have been compiled into a single document. Crucially, the threshold for diagnosing PPH has been adjusted from 500ml of blood loss to 300ml, a shift designed to prompt earlier intervention.
“The new guidelines redefine how postpartum haemorrhage is assessed. Instead of relying on observation alone, the threshold for diagnosing PPH has been reduced from 500ml to 300ml of blood loss. This means that once a woman loses 300ml, the emergency bundle of care must be initiated immediately to prevent complications. The goal is to identify and treat PPH much earlier so mothers do not suffer the consequences of excessive bleeding,” said Prof Obimbo
He believes that if the Ministry of Health fully adopts these guidelines, maternal deaths caused by excessive bleeding, currently around 3,000 annually, could be drastically reduced. Across Africa, the potential impact is even greater, with the possibility of saving up to 56,000 lives every year.
Kenya’s maternal mortality ratio remains high at 355 deaths per 100,000 live births, and specialists agree that with adequate blood and proper adherence to clinical protocols, survival rates can significantly improve.
During a recent stakeholders’ meeting in Nairobi, the PPH Foundation, in collaboration with the University of Nairobi, the Kenya Obstetrical and Gynaecological Society, and the Midwives Association, highlighted the critical importance of public education in languages people understand. They emphasised the need to normalise blood donation and frame it as a shared community responsibility.
They also stressed the urgency of reaching rural and marginalised areas, where the burden of postpartum haemorrhage is equally high, and called for inclusive action involving everyone from the Council of Governors and the private sector to mothers and fathers, to prevent maternal deaths caused by childbirth bleeding.
Postpartum haemorrhage remains one of the deadliest complications of childbirth, claiming the lives of tens of thousands of women every year. Globally, the World Health Organisation estimates that around 70,000 women die annually due to PPH, accounting for more than 20 per cent of all maternal deaths.
The burden is heaviest in sub-Saharan Africa and South Asia, where over 85 per cent of these deaths occur, and nearly 14 million women worldwide experience severe bleeding after childbirth each year.
In Africa, haemorrhage is the leading cause of maternal deaths, with postpartum bleeding responsible for more than 60 per cent of all haemorrhage-related deaths.
Kenya mirrors this trend, where PPH accounts for roughly 40 per cent of maternal deaths. With a maternal mortality ratio of about 355 deaths per 100,000 live births, the country continues to grapple with preventable deaths caused by the lack of timely interventions, including the availability of lifesaving blood transfusions.
Top Stories Today