Why you should seek mental health care- Experts

The most common mental health disorders include; depression, generalised anxiety disorder (GAD), panic disorder, phobias, social anxiety disorder, obsessive-compulsive disorder (OCD) and post-traumatic stress disorder.
Mental illness has long been stigmatised, with many believing that seeking help from a psychologist or psychiatrist implies being "mad" or "crazy," which has discouraged many from getting the assistance they need.
In an interview, some Eastleigh residents revealed a reluctance to seek treatment for conditions like depression or stress. They perceive these issues more as personal mindsets that they can manage independently.
More To Read
- WHO urges countries to protect health budgets amid aid reductions
- ‘Plant trees, not trouble’: Eastleigh official urges unity in climate and crime fight
- Explainer: As mental health challenges rise, here is what you need to know about antidepressants
- Safaricom partners with Eastleigh business community to enhance network and internet connectivity
- Reported massacre at hospital in Sudan’s El Fasher leaves 460 dead
- Mental health advocates call for community-based support as economic strain deepens
John Mwangi, a resident, says he doesn't believe in therapy or consulting a doctor about his mental state. "I prefer to handle my issues on my own."
He acknowledges experiencing stress-inducing situations but claims to manage the pressure independently. "I think people stress themselves out unnecessarily. If you can't handle something, just let it go. Even drinking won't make it disappear," he adds.
Mwangi advocates for not overthinking and believes in resolving his problems alone without confiding in anyone.
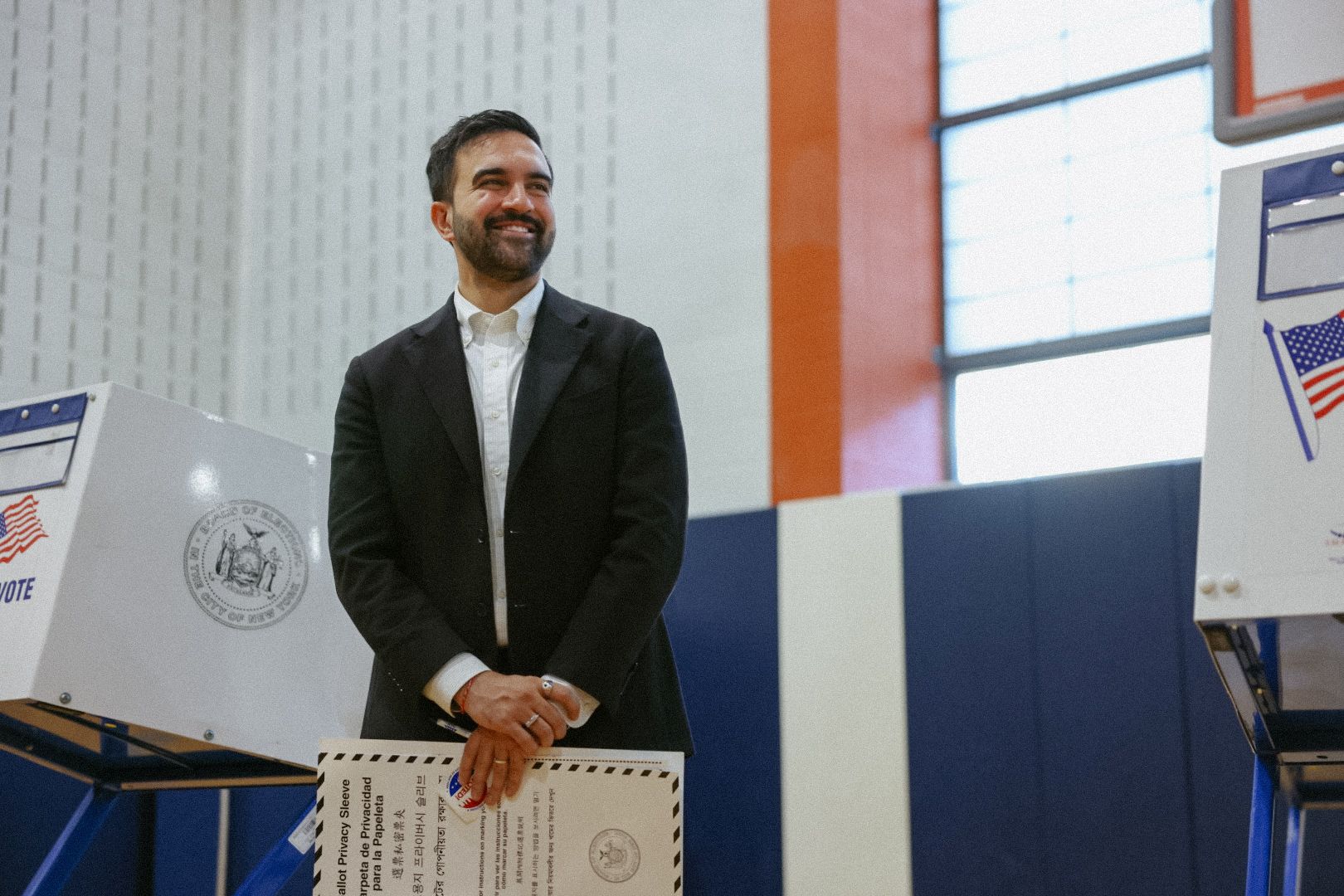
 John Mwangi, a resident, explains how he deals with stress and depression. (Photo: Charity Kilei)
John Mwangi, a resident, explains how he deals with stress and depression. (Photo: Charity Kilei)
Wilson Osoro shares a similar perspective, admitting to lacking awareness about mental health issues. "Stress and depression are normal to me, and I deal with them as they come because what else can I do?"
Osoro acknowledges the stigma surrounding mental health problems. "I think some issues should be kept private, and the idea of talking to someone about them makes me uncomfortable, so I prefer to keep my struggles to myself."
According to Dr Hanaa Muse, a psychologist at Zazi Medical Centre in Eastleigh, many patients lack proper awareness about mental health disorders.
“I've encountered cases where patients are referred to therapy but don't return for further sessions. The myth that seeing a psychologist means you're a crazy person has impeded our treatment efforts,” said Dr Hanaa.
The doctor says that there are numerous cases of mental illnesses, but with proper diagnosis and treatment, patients can recover and regain the ability to function effectively.
"Societal stigma has significantly contributed to the challenges people face, however, we are making progress. Many are gradually embracing therapy," she adds.
Jackline Araya, a clinical social worker at Mathare Teaching and Referral Hospital, says that patients endure a great deal, contending with significant stigma associated with mental health.
“Our community must recognise that mental health conditions are just like any other illness, and they are treatable. With the right medication and support, individuals grappling with these challenges can lead fulfilling lives and function normally,” said Araya.
Araya stresses that full recovery is possible with treatment, citing numerous success stories of patients who have not only regained full functionality but have also been successfully reintegrated into the community, even those who initially had critical disorders.
Other Topics To Read
The most common mental health disorders include; depression, generalised anxiety disorder (GAD), panic disorder, phobias, social anxiety disorder, obsessive-compulsive disorder (OCD) and post-traumatic stress disorder.
 Jackline Araya, a clinical social worker at Mathare Teaching and Referral Hospital. (Photo: Justine Ondieki)
Jackline Araya, a clinical social worker at Mathare Teaching and Referral Hospital. (Photo: Justine Ondieki)
World Health Organisation describes depressive disorder, commonly known as depression, as a prevalent mental health condition characterised by persistent feelings of sadness or disinterest in activities over extended periods and impacts various aspects of life, including relationships with family, and friends, and engagement in the community.
The organisation notes that depression can affect anyone, but individuals who have experienced trauma, significant losses, or stressful events are at a higher risk. Additionally, statistics indicate that depression is more prevalent among women than men.
According to the WHO, globally, an estimated 3.8 per cent of the population experiences depression, with adults representing 5 per cent, including 4 per cent of men and 6 per cent of women. Among adults over 60 years old, the prevalence increases to 5.7 per cent.
WHO highlights that over 280 million people worldwide live with depression, with women being 50 per cent more likely to experience it than men. Furthermore, depression affects more than 10 per cent of pregnant women and those who have recently given birth.
Despite the availability of effective treatments for mental disorders, over 75 per cent of individuals in low- and middle-income countries do not receive adequate care. This deficiency in mental health support is attributed to various barriers, including insufficient investment in mental healthcare, a shortage of trained healthcare professionals, and the pervasive social stigma surrounding mental illness.
The medical professionals stress the significance of seeking treatment for all cases, including depression, which affects a significant portion of the Kenyan population.
According to the Kenyan National Commission of Human Rights, mental health conditions affect between 25 per cent and 40 per cent of outpatients and inpatients.
Among the most common diagnoses in general hospital settings are depression, substance abuse, stress, and anxiety disorders. In a 2017 WHO report, Kenya was ranked fifth among African countries with high rates of depression, with global estimates suggesting that around two million individuals grapple with this condition.
Top Stories Today