Linda Mama budget cut sparks worry over rising risks for pregnant women

Many women are worried as the Treasury has halved the initiative's budget, limiting its benefits to only a few women in marginalised communities.
For about a decade, women from all walks of life have benefited from the Linda Mama programme, which has significantly reduced home deliveries and maternal mortality rates.
Launched in June 2013 by then-President Uhuru Kenyatta, the initiative aimed to alleviate the financial burden on pregnant women, providing services based on need rather than the ability to pay.
More To Read
- Screen time crisis: Experts warn disappearing traditional toys harming children's brains
- Health budget falling short of Abuja Declaration and impact, UHC Healthcare
- Ministry of Health, governors agree to joint audit of UHC staff
- 3,000 ghost workers exposed in UHC payroll scandal amid ongoing strike
- Death of unpaid health worker exposes crisis among UHC staff
- Explainer: Who are the striking UHC workers, and why are they protesting?
This was a major step towards achieving Universal Health Coverage (UHC) in Kenya.
However, many women are now worried as the Treasury has halved the initiative's budget, limiting its benefits to only a few women in marginalised communities. This budget cut threatens to leave countless other women without the support they desperately need.
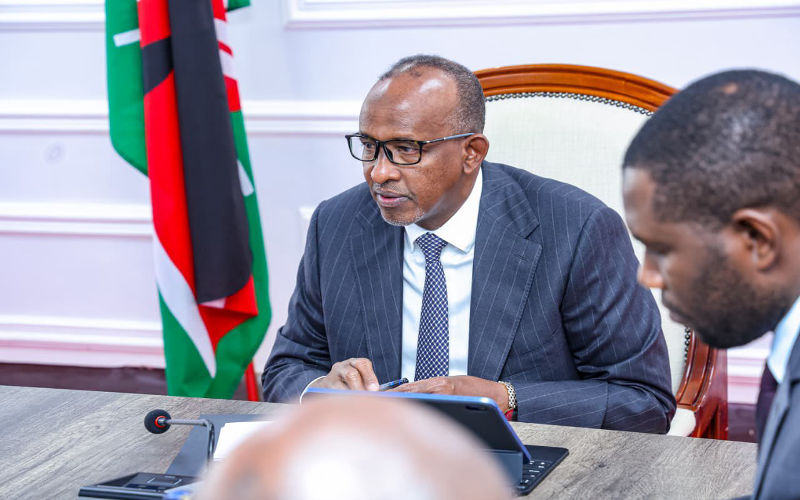
Tom Matiego, a 52-year-old boda boda rider from Eastleigh, Nairobi, said the programme significantly helped his family during a rough patch.
"My wife developed complications and had to be transferred to Kenyatta National Hospital for a C-section. We didn't have any money, but Linda Mama helped us. I didn't have to pay anything," Matiego told The Eastleigh Voice in an interview on Wednesday.
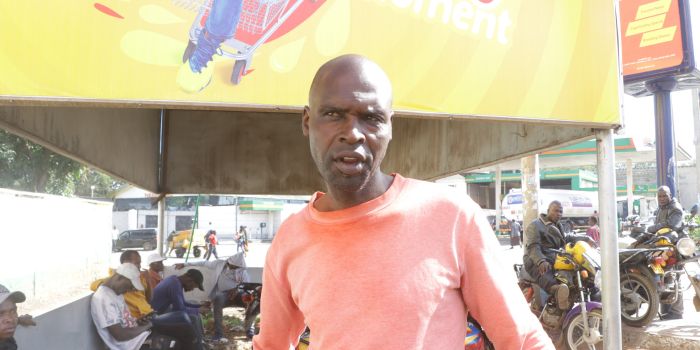 Boda boda rider Tom Matiego, from Eastleigh in Nairobi, speaks to The Eastleigh during an interview on May 22, 2024. (Photo: Justine Ondieki/EV)
Boda boda rider Tom Matiego, from Eastleigh in Nairobi, speaks to The Eastleigh during an interview on May 22, 2024. (Photo: Justine Ondieki/EV)
He was able to focus on providing for his family instead of worrying about a Sh30,000 medical bill.
"This initiative was a lifeline for us. I had no idea how to come up with the money. My plea is for the government to continue this programme because it helps many women and families, especially those who can't afford other medical insurance."
Faith Mwende, a 23-year-old mother from Majengo slum, said she felt hopeful when she conceived, as she didn't have to worry about a medical cover for delivery.
 Faith Mwende, a 23-year-old mother from Majengo slum. (Photo: Charity Kilei)
Faith Mwende, a 23-year-old mother from Majengo slum. (Photo: Charity Kilei)
"I had a safe delivery of my firstborn. I am happy. Being a mother comes with many responsibilities. Linda Mama has been a lifesaver for me and my baby, from all the clinic [checks] to even after delivery."
Gladys Kanini, a 35-year-old mother of four from Majengo, said the programme renewed her hope when I gave birth to her last child.
"Being a hustler and with my husband jobless at the time, there was no way we could have paid for the medical bills," she said.
"In the slums, teenage pregnancy is a common issue. Linda Mama has helped many young girls. The government should reconsider this budget cut because, here in the slum, people just survive. Many girls fall into the wrong hands and end up pregnant. If these services are scrapped, what will become of us?"
She said she earns about Sh100 daily, so it is impossible to save for rent and medical bills.
 Gladys Kanini from the Majengo slum in Pumwani Ward , Nairobi, speaks to The Eastleigh during an interview on May 22, 2024. (Photo: Justine Ondieki/EV)
Gladys Kanini from the Majengo slum in Pumwani Ward , Nairobi, speaks to The Eastleigh during an interview on May 22, 2024. (Photo: Justine Ondieki/EV)
In the 2024/25 budget estimates, the allocation for free delivery services under the Linda Mama initiative, which operates under the now-defunct National Health Insurance Fund (NHIF), was cut from Sh4 billion to Sh2 billion.
This decision has led to a contentious debate between the Ministry of Health and the National Assembly Committee on Health.
Legislators demanded explanations for the budget cut, despite the high demand for delivery services in the country.
Nandi Woman Representative, Cynthia Muge questioned the rationale behind slashing the allocation, citing health data that shows between 6,000 and 8,000 women die every year during delivery in Kenya.
She expressed concern that scrapping the Linda Mama initiative could lead to more deaths.
Further, Kenya records at least 21 neonatal mortalities per 100,000 live births.
The Health ministry says, however, that under the new health scheme, the Social Health Insurance Fund (SHIF), only impoverished women will be considered for free delivery services.
The Linda Mama programme aimed to reduce maternal and infant mortality by providing free delivery services. Since its introduction, the number of hospital deliveries and C-sections has significantly increased.
According to data from the Ministry of Health, registered deliveries rose from 948,000 in 2016 to 1.19 million in 2019.
Before the introduction of free hospital delivery, many women relied on traditional birth attendants, which contributed to high maternal and infant death rates. In 2008/09, Kenya's maternal deaths stood at 488 per 100,000 live births, a number that has since been reduced to 342 per 100,000 live births in 2022.
The Kenya Demographic and Health Report of 2022 says there has been a significant reduction in the number of babies dying at birth over the past five years, with under-five deaths plunging from 52 per 1,000 live births to 41, and infant mortality dropping from 39 per 1,000 live births in 2014 to 32.
According to the World Health Organization (WHO), maternal mortality remains high, with approximately 287,000 women dying during and after pregnancy and childbirth in 2020.
The WHO notes that 95 per cent of these maternal deaths occurred in low- and lower-middle-income countries. Women in low-income countries face a higher lifetime risk of maternal death compared to their counterparts in high-income countries.
The probability that a 15-year-old girl in a low-income country will eventually die from a maternal cause is 1 in 49
The WHO says that most maternal deaths result from complications that arise during pregnancy and childbirth, which are often preventable or treatable with proper medical care.
The major complications responsible for nearly 75 per cent of all maternal deaths include severe bleeding (mostly after childbirth), infections (usually after childbirth), high blood pressure during pregnancy (pre-eclampsia and eclampsia), complications from delivery, and unsafe abortions.
Top Stories Today
- Raila: I do not regret my pact with Ruto
- Heavy rainfall expected across Kenya from Friday, weatherman warns
- Seven Ethiopian migrants die of hunger and thirst after boat engine fails
- Kenya calls for governance overhaul as EAC gridlock deepens
- Court gives IEBC seven days to respond in MPs’ recall petition case
- New Instagram update adds reposts feed, friends tab and Snapchat-style private sharing