Kenya to monitor antibiotics use as resistance threatens effective treatment

According to a 2019 survey by the Institute for Health Metrics and Evaluation, antimicrobial resistance was responsible for approximately 8,500 deaths in Kenya.
Kenya has launched its first comprehensive plan to monitor the consumption of antimicrobial drugs, including antibiotics and antifungals.
This initiative comes in response to the rising trend of drug resistance, which threatens the effectiveness of treatments for various infections.
More To Read
- Pharmacy Board urges Kenyans to report any adverse drug reactions amid spike in cases
- Malaria fight at risk as drug resistance spreads despite new tools saving millions
- Malaria: Drug resistance and underfunding threaten progress towards eliminating killer disease
- Kenya reports first local case of powerful drug-resistant bacterial gene
- WHO warns of rising antimicrobial resistance in fungal infections
- Ministry warns Kenyans on escalating antibiotic resistance
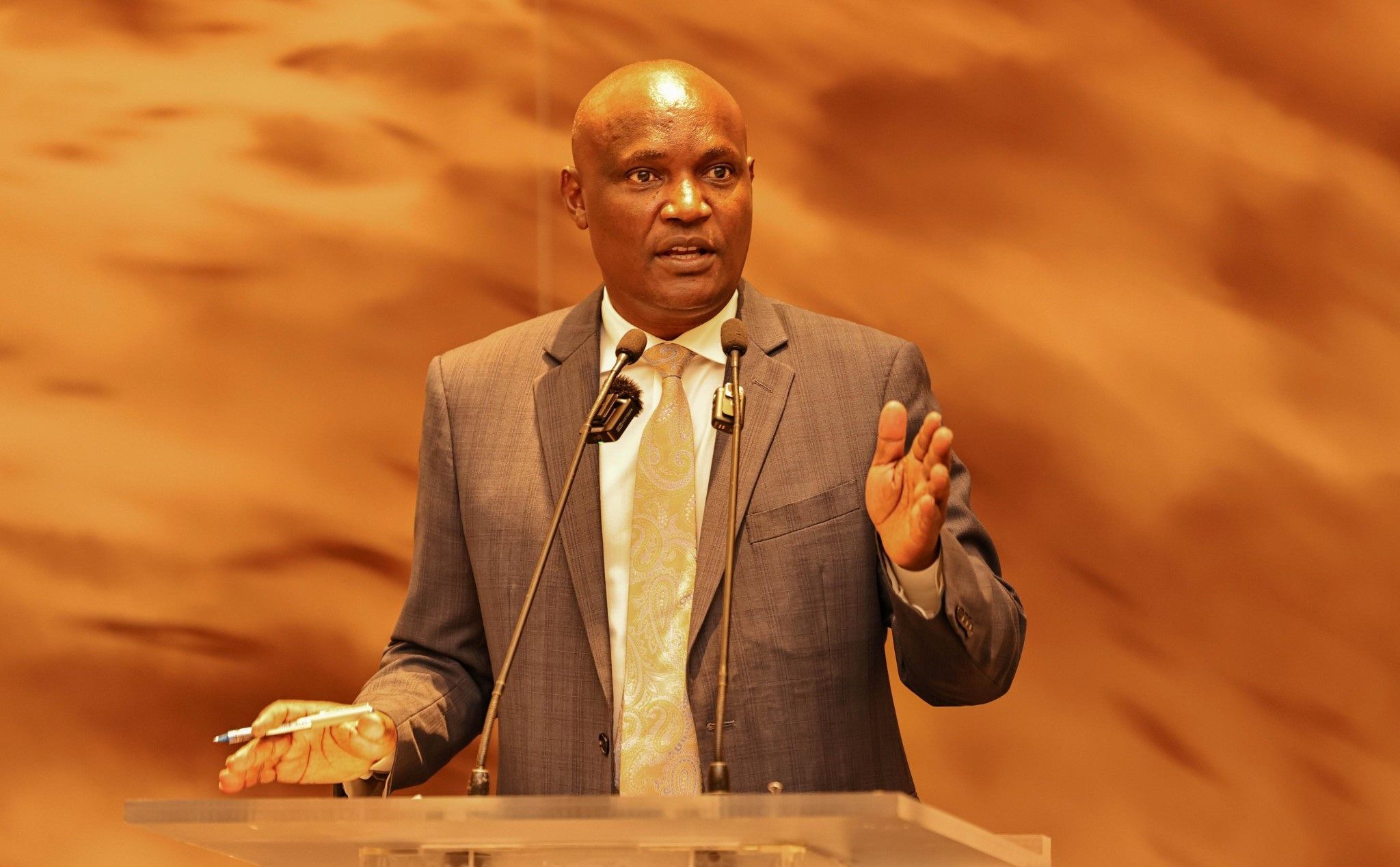
The Kenya Surveillance System for Antimicrobial Consumption was introduced in Nairobi by the Pharmacy and Poisons Board (PPB).
Dr Fred Siyoi, the head of PPB, said that until now, Kenya lacked a national system to track antimicrobial use.
He noted that effective surveillance is essential for understanding consumption patterns and their link to resistance trends.
"If left unchecked, antimicrobial resistance has the potential to reverse decades of medical progress, leaving us vulnerable to infections that were once easily treatable," he warned.
Antimicrobial resistance (AMR) occurs when microorganisms evolve and become resistant to drugs designed to eliminate them, complicating the treatment of common infections like pneumonia, tuberculosis, and malaria.
Deaths
According to a 2019 survey by the Institute for Health Metrics and Evaluation, AMR was responsible for approximately 8,500 deaths in Kenya.
The new system will enable the PPB to collect, analyse and interpret data on antimicrobial use across the entire pharmaceutical supply chain, from importers and manufacturers to pharmacies and healthcare facilities.
"Kenya will gain a clearer picture of antimicrobial consumption trends, enabling us to target interventions more effectively, reduce irrational antimicrobial use, and ultimately protect the health of our population," Siyoi stated during the launch of the online platform.
Dr Karim Wanga, a regulatory officer at PPB, identified indiscriminate use, misuse, and overuse in humans, animals, and the environment as primary drivers of AMR.
He also highlighted poor disposal practices and the presence of antimicrobials in the environment as contributing factors.
"Global deaths from drug-resistant infections are projected to increase from the current 700,000 to 10 million annually," Wanga said.
The next phase of the initiative will involve training and sensitising local manufacturers, importers, distributors, and community pharmacies about the new system.
Wanga noted that the rollout will require significant resources.
Crucial insights
Dr Rosemary Njogu, another regulatory officer at PPB, stated that data from this system will provide healthcare professionals and policymakers with crucial insights into antimicrobial drug consumption trends, helping to inform national action plans against AMR.
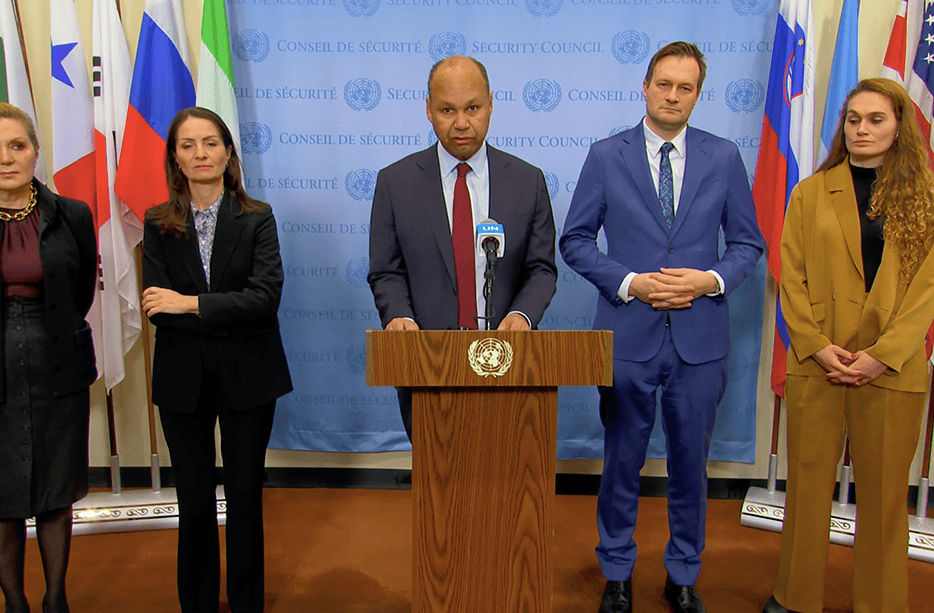
In September, global leaders at the 79th UN General Assembly endorsed a political declaration on antimicrobial resistance, which set targets to reduce the estimated 4.95 million human deaths associated with bacterial AMR annually by 10 per cent by 2030.
While political declarations are not legally binding, they carry significant weight.
The declaration called for sustainable national financing and Sh12.9 billion in catalytic funding to help achieve a target of at least 60 per cent of countries implementing funded national action plans on AMR by 2030.
Diversify funding
This goal aims to diversify funding sources and attract more contributors to the Antimicrobial Resistance Multi-Partner Trust Fund.
Inger Andersen, executive director of the United Nations Environment Programme (UNEP), acknowledged the declaration's importance.
"Evidence is mounting that the environment plays a significant role in the development, spread, and transmission of AMR, including transmission between humans and animals," she said.
"That is why if we're to reduce the burden of AMR and its risks, the environment must be part of the solution," Andersen added.
On the human health front, the declaration sets an ambitious target: at least 70 per cent of antibiotics used globally for human health should belong to the WHO Access group, which features drugs with minimal side effects and lower potential to cause AMR.
Top Stories Today