‘We do everything, but get nothing’: Kenyan nurses tell of pay gaps, exploitation and burnout

Pay disparities and poor treatment continue to plague healthcare workers under the UHC programme, with around 8,500 staff reportedly earning only half their salaries for over five years since the Covid-19 pandemic.
For Gloria*, a nurse and health assistant working in various private healthcare facilities in Kenya, every day begins before dawn and ends long after sunset.
Despite her qualifications and years of experience, her reality is one of overwork, underpayment, and a persistent fight to be treated with fairness and dignity.
More To Read
- Extreme weather affects mental health: what vulnerable women in Kenya told us
- Extreme weather affects mental health: What vulnerable women in Kenya told us
- Study links early smartphone use to severe mental health outcomes in young adults
- Mentally ill mother sentenced to three years probation for killing six-month-old baby
- ‘They told them I was dead': A mother’s pain and the mental toll of family separation on children
- Nursing internships suspended as Ministry of Health orders audit over fake postings
She doesn’t just attend to patients. On some days, she doubles as a lab assistant. Other times, she steps in for the pharmacist. Her role is constantly shifting to fill the gaps in understaffed facilities, but her pay never reflects these added responsibilities.
“I do everything,” she says. “But I’m paid like I’m only doing the basics.”
Gloria has brought up the issue of poor pay and inflexible shifts with her supervisor numerous times, especially as the demands of the job have begun to take a toll on her mental and physical health. Still, nothing changes.
“I’ve raised these concerns again and again, but I’m always met with the same response: ‘You should be grateful to have a job.’ It’s like our struggles don’t matter because someone else out there is unemployed.”
Relief nurse shock
But one incident shifted her frustration into something more urgent. A relief nurse was recently brought in to take over some of her night shifts. Gloria assumed he was there temporarily and didn’t think much of it—until she discovered he was being paid twice what she earns.
“I was shocked,” she recalls. “He was just covering for a few nights, and yet he earned double my salary. I’ve been here for years, and I’ve had to beg just to be heard.”
When she inquired, she found that the nurse hadn't even negotiated his pay—that was simply the offer. The realisation was deeply demoralising.
“That’s when I truly understood how little they value us, not just as nurses, we do the work, carry the load, and still get the scraps.”
Gloria has considered quitting many times, but jobs are scarce, and every attempt to find better opportunities in Kenya has led to disappointment. Like many others, she’s now focused on one goal: leaving the country.
“If I get the chance to go abroad, I won’t think twice,” she says firmly. “I’m just a placeholder here. When something opens up, I’m gone.”
Her story is far from unique.
Across Kenya, many female nurses share similar experiences: overworked, underpaid, and passed over.
Idah, another nurse, has been working as a reliever for over two years, hoping for a permanent contract. But despite her persistence and qualifications, she remains in a precarious position—called in last-minute, paid less, and given fewer shifts than her counterparts
“We have the same qualifications,” she says, “but the men get better shifts, more flexibility, and are paid more. It’s like they’re automatically treated better.”
Worse still, Idah reveals the exploitation some women face just to secure shifts.
“Some of us are asked for sexual favours to get a slot. If you say no, you’re sidelined—you get no work.”
She recalls months when she worked for only six days out of 30, despite being available. When she questioned this, she was told there was a “budget cut”, a vague and inconsistent explanation.
Summoned at any time
As a reliever, Idah can be summoned at any time, day or night, and is expected to show up, no matter the circumstances.
“You can be ignored for weeks, then suddenly get a call at 1 am. If you don’t go, it counts against you,” she says. “It’s like we’re always on edge.”
Kenya’s nursing workforce is largely composed of women, yet the profession is built on systemic inequality.
Under temporary contracts, especially those tied to Universal Health Coverage (UHC) programmes, nurses can earn as little as a quarter of the standard government salary, despite carrying similar workloads.
In Kenya, women make up about 70 per cent of the healthcare workforce and 80 per cent of nurses and midwives, yet they are underrepresented in leadership. While they hold over 70 per cent of mid-level roles, only 42 per cent occupy top leadership positions.
Factors like low pay, poor working conditions, gender-biased policies, and cultural norms limit their career progression. Despite their numbers, women face systemic barriers to advancement, reflecting a global trend.
The issue isn’t just about wages—it’s about respect, safety, and opportunity.
Meanwhile, as more Kenyan nurses leave the country in search of better conditions abroad, the local health system suffers. Hospitals and clinics are left with critical staffing shortages, and the cycle of overwork and exploitation only deepens for those who remain.
Working abroad
Each year, over 800 Kenyan nurses leave the country, most heading to the United States, Canada, or the United Kingdom, according to the Kenya National Union of Nurses. This steady outflow is part of a broader trend within the global healthcare labour market, and it comes at a significant cost to the country’s health system.
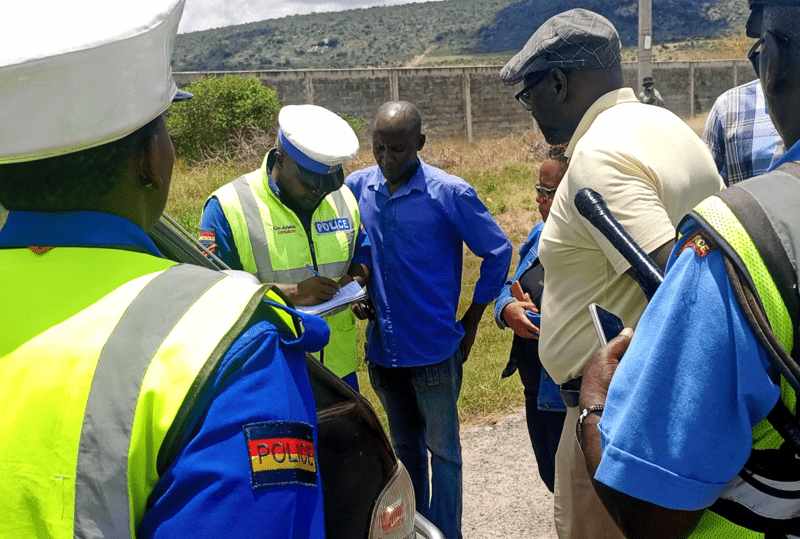
Pay disparities and poor treatment continue to plague healthcare workers under the UHC programme, with around 8,500 staff reportedly earning only half their salaries for over five years since the Covid-19 pandemic. Many have yet to receive their gratuity, despite serving in high-risk conditions.
Among them are approximately 2,500 nurses hired under the UHC initiative in 2020. The Ministry of Health now intends to transfer their payroll to county governments, but the terms remain unclear, particularly whether future payments will align with the Salaries and Remuneration Commission (SRC) guidelines. This ongoing uncertainty has driven many nurses to prolonged street protests.
The World Health Organisation’s latest report notes that leadership development opportunities within the nursing workforce remain uneven across countries.
Nursing leadership
Although 66 per cent of countries report having initiatives to support nursing leadership, only 25 per cent of low-income countries offer structured leadership development programmes. This gap highlights persistent inequities in professional advancement opportunities for nurses, particularly in resource-constrained settings.
Gender and equity also remain central concerns.
Women continue to dominate the nursing profession, representing 85 per cent of the global nursing workforce. Despite overall growth—from 27.9 million nurses in 2018 to 29.8 million in 2023—there are still wide disparities in nurse availability across regions and countries. These imbalances leave many populations without access to essential health services and threaten progress toward UHC, global health security, and health-related development goals.
International migration plays a significant role in shaping the nursing workforce.
One in seven nurses worldwide is foreign-born, with the figure rising to 23 per cent in high-income countries.
By comparison, foreign-born nurses account for only 8 per cent in upper-middle-income countries, 1 per cent in lower-middle-income countries, and 3 per cent in low-income countries, revealing a significant reliance on international recruitment in wealthier nations.
Mental health and workforce well-being continue to be areas of concern.
Despite the increased workload, stress, and trauma nurses have faced during and after the Covid-19 pandemic, only 42 per cent of responding countries report having provisions in place to support the mental health of nurses.
Top Stories Today