Mothers' battle for survival when diabetes complicates pregnancy

Dr Ester Mwaura stresses that managing diabetes during pregnancy requires close monitoring to prevent complications. She urges expectant mothers to attend regular prenatal clinics, as early detection and proper management are essential for both maternal and foetal health.
For many women with diabetes, the fear of slow-healing wounds lingers like a dark cloud, especially during childbirth.
Pauline* knew this fear all too well. Having battled diabetes for decades, she was no stranger to its challenges, but nothing prepared her for what she faced when she gave birth to her third child.
More To Read
- How follow-up programmes bridge treatment gap in non-communicable diseases
- Governors sound alarm as 934 newborns die amid funding row in health sector
- Born too soon: The hidden burden of preterm birth, fight for survival
- Study shows women under 50 face higher risk of colon growths from ultra-processed foods
- WHO issues first global guidelines on diabetes in pregnancy
- Governors decry Health Ministry’s move to deny maternity funds to dispensaries
Now 57, she recalls how different this pregnancy was from her first two. While both had required caesarean sections, they were relatively smooth. This time, everything felt harder. Her appetite dwindled, making it difficult to follow her diet and medication. Each passing day was a struggle, and by the time she went into labour, she was exhausted.
After yet another C-section, things took a turn for the worse. Her newborn had trouble breathing and was rushed to the ICU. As if that were not enough, he developed jaundice. Pauline watched helplessly as her baby fought for his life, all while battling her post-surgery complications.
“I was not only frustrated but deeply depressed. I longed to hold my baby, yet my wound refused to heal. It took nearly three months, and the sutures did not hold. I had to be taken back to the theatre for repair.”
The healing process was painfully slow. Her surgical wound remained stubbornly open. To make matters worse, her poor appetite meant she struggled to take her medication as prescribed. Doctors placed her on insulin injections twice a day, but every shot left her in pain. Her thighs became too sore, so they switched to her lower abdomen, but the discomfort did not ease.
“The injections became unbearable. My thighs were swollen and tender, so we moved to my lower stomach, but every push of the needle sent sharp pain through me. At the same time, I was losing so much weight, and my baby was not getting better. On top of that, my body was not producing enough milk—how could I feed my child?”
Pauline’s biggest challenge was food. Hospital nutritionists experimented with different ways to make her meals more appealing, but nothing worked. Constipation became another battle, and when she tried to manage it without laxatives, her wound reopened. She felt trapped in an endless cycle of pain and exhaustion. Despite her efforts, her blood sugar levels refused to drop below the recommended.
Desperate to regain her strength, she joined a gym, but even exercise could not lift her spirits. By the time she and her baby were discharged after a long hospital stay, she felt no joy in returning home. She was weak, her skin was pale and dry, and her feet cracked painfully with each step. Emotionally, she was just as fragile.
Determined to find relief, Pauline turned to herbal medicine. The concoctions triggered severe diarrhoea, but surprisingly, her appetite returned. However, her surgical wound remained sore, a lingering reminder of the battle her body was still fighting.
Then, during a routine check-up, her doctor made a strange recommendation—he advised her to drink a glass of Guinness beer before bed every night. At first, she dismissed the idea. Alcohol was never part of her routine. But as exhaustion wore her down, she decided to give it a try.
“To my surprise, I started sleeping better. My metabolism improved, and for the first time in a long while, I felt like myself again. Encouraged, I even went back to school to pursue my master’s degree. But after a year, I stopped taking the beer.”
Just when she thought she had overcome the worst, another nightmare unfolded—her baby stopped feeding well and became restless. Alarmed, she took him for tests. The results shattered her world: her child had diabetes.
“By this time, I had developed a deep mistrust of hospitals. I started questioning everything. I suspected that big pharmaceutical companies and doctors were in business together—creating conditions, then profiting from them. I felt trapped in a system that was designed to make money off people like me. So I stopped taking my medication.”
Disillusioned and overwhelmed, she turned her back on treatment. But with time, she came to accept the reality of her condition. Now, she dedicates her time to encouraging other women with diabetes, especially those navigating pregnancy.
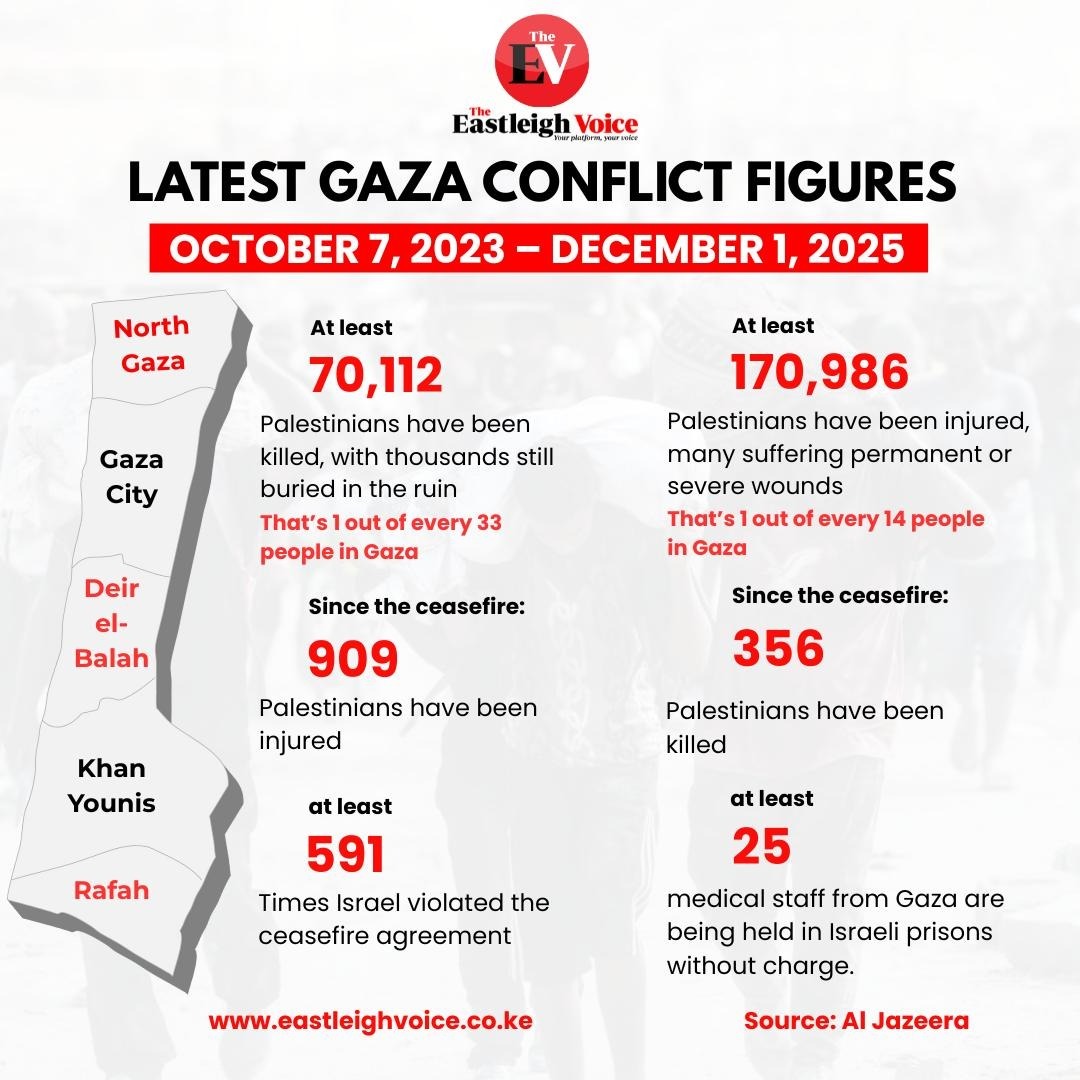
 Njeri Kimani narrates her painful journey with diabetes during pregnancy. (Handout)
Njeri Kimani narrates her painful journey with diabetes during pregnancy. (Handout)
Pregnancy complications
For many expectant mothers, an ultrasound is a moment of excitement—a chance to see their baby kicking and growing. But for Njeri Kimani, that moment was filled with shock. Her doctor told her that her baby was bigger than expected, a common complication for mothers with diabetes.
Njeri’s journey with Type 1 diabetes began in 2022, a diagnosis that changed her life. At first, she managed well, sticking to her insulin routine and carefully monitoring her blood sugar levels. But everything shifted when she became pregnant in 2024. Suddenly, what had once been manageable became a daily battle for survival.
During pregnancy, Njeri’s blood sugar levels skyrocketed, reaching dangerous highs of 30 mmol/L. She felt like she was on the brink of collapse.
"At first, everything seemed fine," she recalls. "Then, after discovering I was pregnant, my sugar levels shot up, and I felt like I was dying. I had no choice but to become extra cautious and check my sugar levels constantly."
Before pregnancy, insulin alone was enough to control her diabetes. But now, her doctors added Glucophage to her regimen. Every day became a balancing act of measuring sugar levels, adjusting her diet, and battling pregnancy cravings.
Njeri worked closely with both her gynaecologist and diabetes specialist to ensure that her condition was well managed. But despite her efforts, complications arose. Her baby was growing at an accelerated rate, and doctors warned her about excessive amniotic fluid. By the time she reached 38 weeks, her baby weighed 4.1 kilograms, making a C-section the safest option.
One of the biggest challenges Njeri faced was the financial burden of managing diabetes during pregnancy. Without private insurance, the cost of care quickly became overwhelming. Every visit to the diabetes clinic required at least Sh10,000, and by the end of her pregnancy, she had spent over Sh85,000 on medical expenses alone.
Early detection
Dr Ester Mwaura stresses that managing diabetes during pregnancy requires close monitoring to prevent complications. She urges expectant mothers to attend regular prenatal clinics, as early detection and proper management are essential for both maternal and foetal health.
Diabetes during pregnancy does not just affect the mother—it also poses serious risks to the baby. One of the most common complications is macrosomia, where the baby grows excessively large due to high sugar levels in the womb. Another major concern is neonatal hypoglycaemia, where the baby’s blood sugar drops dangerously low after birth.
Dr Mwaura emphasises that early diagnosis and proper management can significantly reduce these risks. "We advise women to check their sugar levels frequently, maintain a balanced diet, and take insulin as prescribed if necessary."
Above all, routine prenatal check-ups should never be skipped. "These visits allow us to monitor both the mother and baby’s health and adjust treatment when necessary," Dr Mwaura advises.
With proper care and discipline, women with diabetes can still experience a safe and healthy pregnancy.
Top Stories Today