Private hospitals give Duale two weeks to settle NHIF arrears

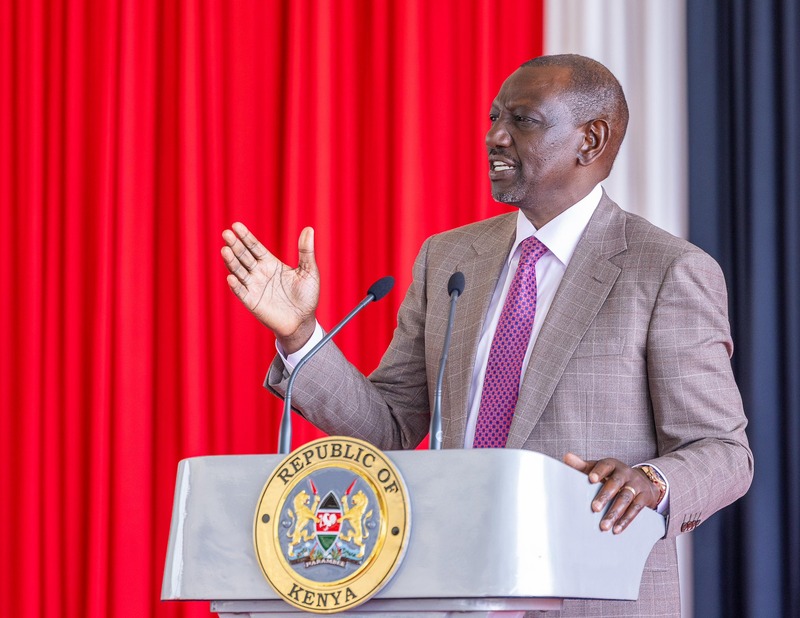
Rural and Urban Private Hospitals Association of Kenya (RUPHA) said the government had failed to honour President William Ruto’s March 5 directive to pay facilities owed Sh10 million or less in full, and to carry out a structured verification process for larger claims.
Private hospitals have given Health Cabinet Secretary Aden Duale until September 9 to clear pending National Health Insurance Fund (NHIF) arrears, warning that continued delays are crippling service delivery.
In a statement dated August 14, the Rural and Urban Private Hospitals Association of Kenya (RUPHA) said the government had failed to honour President William Ruto’s March 5 directive to pay facilities owed Sh10 million or less in full, and to carry out a structured verification process for larger claims.
More To Read
- Counties urged to ditch costly overseas benchmarking tours amid fiscal constraints
- Kenya’s primary healthcare crisis: Patients struggle despite ‘free’ treatment, SHA registration
- High Court quashes Aden Duale's NHIF pending bills verification committee
- Senate faults SHA over delayed Sh8 billion payment to families of deceased civil servants
- Over 23 million Kenyans registered for SHA, but more than 17 million aren’t contributing to the fund
- Private hospitals blame flawed SHA model as 40 facilities face suspension
RUPHA said that 162 days after the directive, no public, private or faith-based healthcare facility had received payment.
“We write to express our deep concern regarding the continued delay in the fulfilment of the Presidential directive issued on March 5 regarding the settlement of NHIF pending bills. As of August 14, it has been 162 days, more than five months, since this directive was issued, yet no healthcare facility has received any payment for the NHIF arrears it is owed,” the statement signed by board member Miriam Wanjiku read.
The payment process was thrown into disarray in July when the High Court in Eldoret declared the NHIF Pending Bills Verification Committee unconstitutional.
The court ruled that the Social Health Insurance Act lacked transitional provisions to allow such a committee, and that any verification involving patient data had to follow proper legal guidelines.
The committee, gazetted on March 28, had been tasked with reviewing claims submitted between July 2022 and September 2024.
With its dissolution, thousands of claims remain pending, leaving hospitals without a clear path to reimbursement.
Speaking on July 8, Duale said the National Treasury had allocated Sh5.3 billion to settle NHIF claims of Sh10 million and below. However, RUPHA says it will no longer rely on verbal assurances and now wants a written guarantee that payments will be made by September 9.
“We ask that you issue a formal written commitment to all providers confirming that verified NHIF claims of Sh10 million and below will be settled on or before 9th September 2025, as earlier promised,” the statement added.
The association has also asked Duale to instruct the Social Health Authority (SHA) to publish the pending claim amounts per facility earmarked for payment within the two-week deadline, and to immediately pay uncontested liabilities for hospitals that completed the NHIF-led verification process in 2023/2024.
RUPHA further wants the SHA to revive its internal branch-led claims verification process for facilities that missed the earlier NHIF sign-off, and to complete it within three months.
While reiterating its willingness to work with the Ministry of Health, RUPHA said resolving the arrears was urgent to restore working capital in the health sector and support the Universal Health Coverage agenda under the Taifa Care framework.
Top Stories Today