No active Mpox cases in Kenya, Ministry of Health announces

Health experts fear that the true extent of the Mpox outbreak may be significantly underreported due to insufficient diagnostics and testing in many regions.
There are no active cases of Mpox in the country following the complete recovery of the initial case identified on July 29, according to the Ministry of Health.
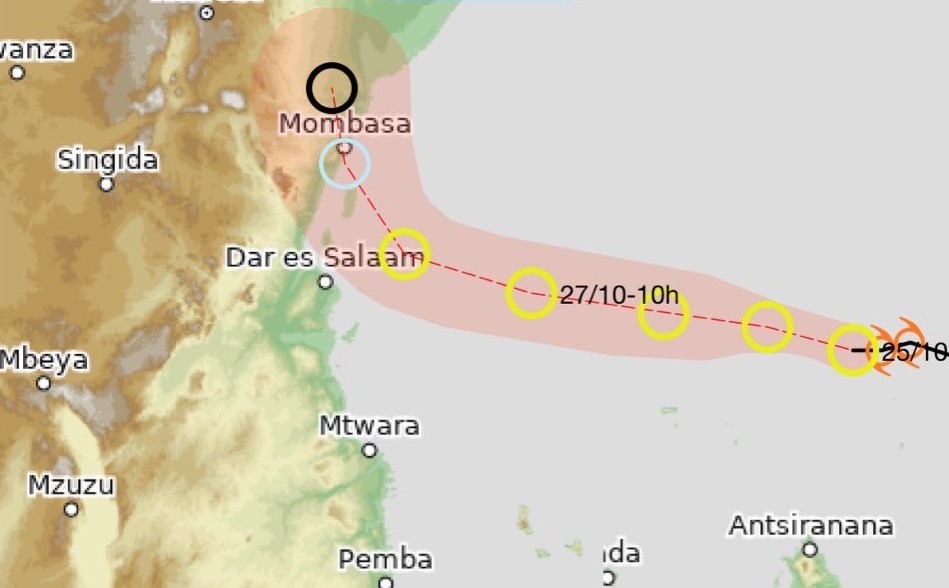
Health CS Debora Mulongo on Friday confirmed the full recovery of the sole reported case, involving an individual who travelled from Kampala, Uganda, to Mombasa and then proceeded to Rwanda via Tanzania's Taita Taveta border point.
More To Read
- Severe flooding affects over 960,000 in South Sudan: UN
- WHO says polio eradication still feasible despite Sh219 billion funding cuts
- Namibia declares mpox outbreak after confirmed case in Swakopmund
- WHO says DRC could declare end of Ebola outbreak by December
- Last Ebola patient discharged as WHO starts countdown to end DRC outbreak
- WHO raises alarm as antibiotic resistance threatens global health gains
"We have screened twelve individuals who came into contact with the initial case, as well as an additional six suspected cases, all of whom tested negative for Mpox. There have been no new confirmed cases since the first one," said Mulongo.
To curb the spread of Mpox, the MoH has screened more than 250,000 Kenyans and travellers at all ports of entry since confirming the case two weeks ago. This comprehensive screening initiative is part of a broader strategy to prevent further transmission of the virus within the country.
"We have screened 250,000 travellers so far, and no suspected Mpox cases were detected through these screenings. We have also activated all 26 public health emergency operations centres nationwide, prepared laboratories for Mpox testing, and deployed 120 trained personnel to manage any potential outbreak,” reported Mary Muthoni, Principal Secretary of Public Health and Professional Standards.
Apart from the initial case reported on July 31, 2024, no other cases have been detected, and contact tracing is ongoing. The Ministry emphasised that these measures are critical to swiftly identifying new cases and ensuring the virus does not spread further.
Kenya's response includes enhanced nationwide surveillance, activation of Public Health Emergency Operation Centres and Incident Management Teams, ongoing advisories to healthcare workers on detection and management, and public sensitisation efforts to raise awareness about Mpox risks and preventive actions.
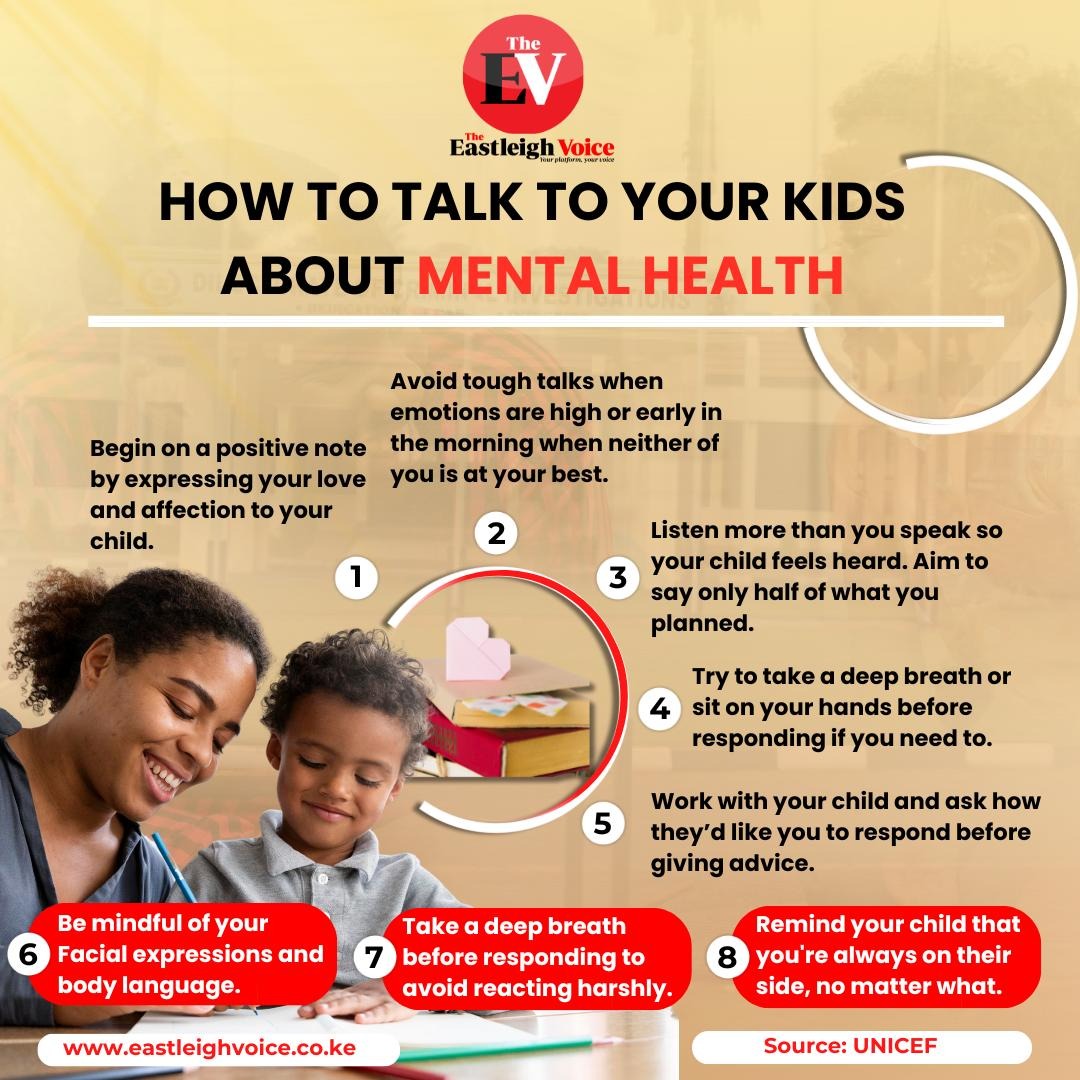
The Ministry advises the public to practice regular handwashing with soap and water or use alcohol-based hand sanitisers, as well as to avoid contact with people showing Mpox-like symptoms.
The ministry has urged Kenyans to visit medical facilities if they experience symptoms and to take necessary precautions.
Public health emergency
Both the Africa Centre for Disease Control and Prevention and the World Health Organisation have declared Mpox a public health emergency, highlighting its significance as a public health concern for the second time.
“We remain vigilant and continue to monitor the situation closely. Our priority is to ensure the health and safety of all Kenyans,” stated Mulongo, reaffirming the government's commitment to public health.
Mpox, formerly known as monkeypox, is a rare viral disease caused by the Mpox virus, which belongs to the same family of viruses as smallpox. Initially identified in monkeys, it primarily affects rodents and other animals, with humans contracting it through contact with infected animals or contaminated materials.
The disease commonly causes rashes, lesions, and pain, which can be managed with supportive care to ease symptoms and avoid complications. While treatments are limited to some countries, most people recover within a month. However, some cases can lead to severe illness or death. The current outbreak in eastern DRC is due to a new variant, clade 1b, which causes more severe illness than clade 2.
According to the Africa Centres for Disease Control and Prevention (Africa CDC), there were 8,376 Mpox cases recorded in Africa in January 2022. By 2023, the number had increased to 14,957, and between January and August 2024, the cases spiked further to 15,132. The total number of deaths has reached 1,456.
Other Topics To Read
The WHO's declaration was made by its Director General, Dr. Tedros Ghebreyesus, following consultations with its emergency committee. Kenya, Burundi, Uganda, and Rwanda have reported a more virulent strain of the virus, named clade 1b, marking the first time these countries have encountered the disease.
"Today, the Emergency Committee on Mpox met and advised me that, in its view, the situation constitutes a public health emergency of international concern. I have accepted that advice," stated Dr. Tedros. "WHO is on the ground, working with the affected countries and others at risk through our country and regional offices, as well as with partners, including NGOs and civil society."
WHO’s declaration
The WHO’s declaration under the International Health Regulations indicates an "extraordinary event that constitutes a public health risk to other states through the international spread of disease and requires a coordinated international response." The organisation explained that this status implies a "serious, sudden, unusual, or unexpected situation, carrying implications for public health beyond the affected state’s national border, and may require immediate international action."
Health experts fear that the true extent of the Mpox outbreak may be significantly underreported due to insufficient diagnostics and testing in many regions.
Dr. Matshidiso Moeti, WHO Regional Director for Africa, emphasised the importance of a coordinated international effort to control the outbreak. "With the growing spread of the virus, we’re scaling up further through coordinated international action to support countries in bringing the outbreaks to an end," he said.
In response to the emergency, WHO is appealing for Sh1.95 billion (US$15 million) to support surveillance, preparedness, and response activities. It has already released Sh185 million (US$ 1.45 million) from its Contingency Fund for Emergencies to enable an immediate scale-up of operations. Additionally, WHO has issued an urgent call for vaccine manufacturers to submit an Expression of Interest for Emergency Use Listing (EUL) of Mpox vaccines.
The Africa CDC recommends two vaccines for use against Mpox: JYNNEOS and ACAM2000. JYNNEOS, a two-dose vaccine series administered four weeks apart, is preferred for the current outbreak.
"The JYNNEOS vaccine does not cause Mpox, smallpox, or any significant adverse reaction. Indications for the vaccine include known and presumed contacts of a case of Mpox and queer individuals who have had multiple sexual partners in the last 14 days," says Africa CDC.
Vaccination is crucial for preventing Mpox, particularly among high-risk populations such as healthcare workers, immunocompromised individuals, and sex workers. The Africa CDC advises post-exposure prophylaxis (PEP) with the approved vaccine for all close contacts of confirmed cases, including those living in the same household, sexual partners, and individuals who have come into contact with the patient’s rashes.
Top Stories Today