WHO flags Hepatitis D as carcinogenic, raises liver cancer alert
Viral hepatitis is now the second-deadliest virus globally, after COVID-19, affecting over 300 million people and causing more than 1.3 million deaths every year, primarily due to liver cirrhosis and cancer.
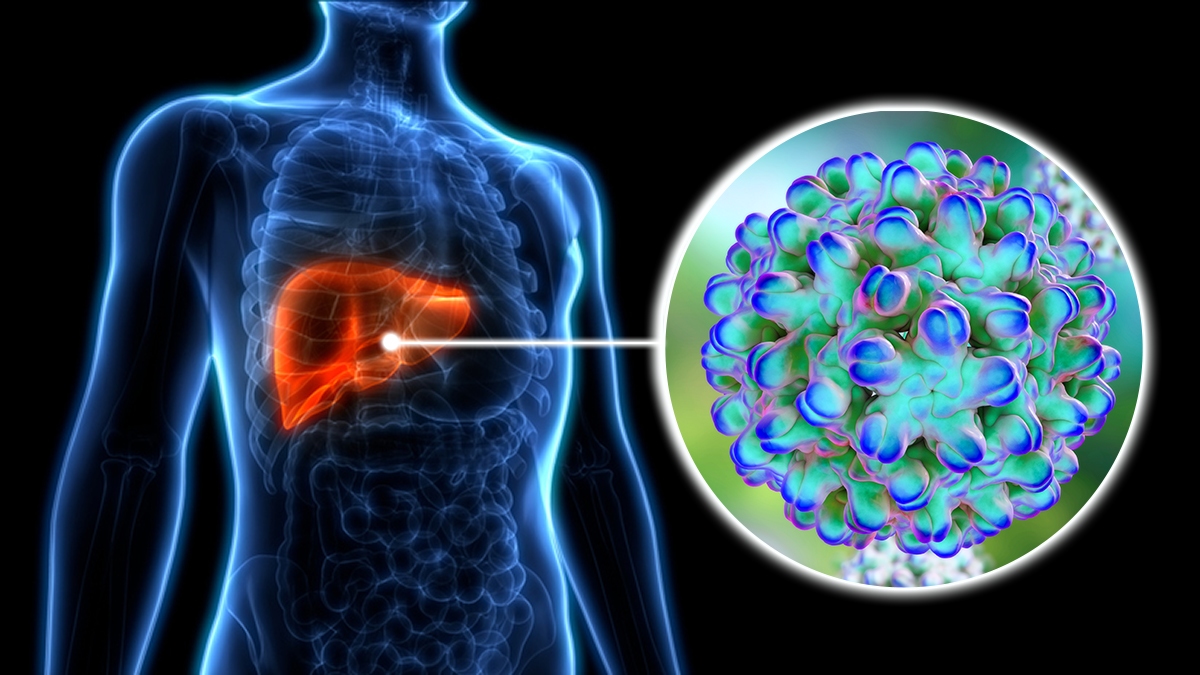
The World Health Organisation (WHO) has declared Hepatitis D as carcinogenic, meaning it can cause cancer in humans.
The virus, which only affects individuals already infected with Hepatitis B, is now recognised to be associated with a two- to six-fold higher risk of liver cancer compared to Hepatitis B alone.
More To Read
- Viral infections linked to higher risk of heart attacks and strokes
- Unmasking hepatitis: The five types, their causes and treatment
- Kenyan mother’s brave battle with hepatitis B: From liver cancer to a life-saving transplant
- Mombasa's methadone clinic to relocate over security concerns
- Hepatitis B: The overlooked health crisis silently spreading across Kenya and Africa
- Somalia issues nationwide alert as hepatitis cases surge
“This reclassification marks a critical step in global efforts to raise awareness, improve screening, and expand access to new treatments for hepatitis D,” stated WHO, urging nations to act fast in preventing a growing crisis of liver-related illnesses.
The decision follows an earlier classification by the International Agency for Research on Cancer (IARC), a United Nations body, which had also labelled Hepatitis D as carcinogenic, placing it in the same category as Hepatitis B and C.
Viral Hepatitis: A silent killer
According to WHO, viral hepatitis types A, B, C, D, and E are major causes of acute liver infection. Among these, only hepatitis B, C, and D can lead to chronic infections that significantly increase the risk of cirrhosis, liver failure, or liver cancer.
Viral hepatitis is now the second-deadliest virus globally, after COVID-19, affecting over 300 million people and causing more than 1.3 million deaths every year, primarily due to liver cirrhosis and cancer.
“Every 30 seconds, someone dies from a hepatitis-related severe liver disease or liver cancer. Yet we have the tools to stop hepatitis,” said Dr Tedros Ghebreyesus, WHO Director-General.
The World Hepatitis Alliance adds that many of those infected are unaware of their condition, allowing the disease to progress unchecked.
The dangerous duo: Hepatitis B and D
Hepatitis D (HDV) cannot infect individuals without the presence of the hepatitis B virus (HBV). It is considered a satellite virus, and co-infection can cause severe liver inflammation, rapid progression to cirrhosis, and significantly increase the risk of liver cancer.
Typical symptoms of hepatitis D infection, which appear 3–7 weeks post-infection, include fever, fatigue, jaundice, nausea, dark urine, and right upper quadrant pain, a sign of liver involvement.
Prevention and treatment
According to the WHO, the key to preventing Hepatitis D lies in Hepatitis B vaccination. To prevent HDV, one must be vaccinated against the HBV virus. The HBV vaccination protects against hepatitis B infection, thereby preventing hepatitis D infection and related cancer.
WHO has published new guidelines on testing and diagnosis of both Hepatitis B and D in 2024 and continues to track the progress of innovative treatments.
“The full benefit of reducing liver cirrhosis and cancer deaths can only be realised through urgent action to scale up and integrate hepatitis services—including vaccination, testing, harm reduction, and treatment—into national health systems,” noted Dr Meg Doherty, WHO’s incoming Director of Science for Health.
Hepatitis C can now be cured within 2–3 months using oral medicines, and hepatitis B can be effectively suppressed with lifelong therapy. However, treatment options for hepatitis D are still evolving.
In Kenya, the Ministry of Health has intensified efforts to combat the growing threat of viral hepatitis, citing increasing infection rates and low levels of public awareness, especially in rural communities.
Speaking in Mombasa during this year’s World Hepatitis Day commemoration, Director General for Health Dr Patrick Amoth revealed that an estimated three per cent of Kenyans are living with Hepatitis B and C, with the majority of cases remaining undiagnosed due to limited knowledge and access to testing services.
“In many parts of the country, especially in rural areas, people are simply unaware of the risks and symptoms associated with hepatitis,” said Dr Amoth.
Also, the government has now rolled out free treatment for both Hepatitis B and C.
“The government is covering the cost of treatment, meaning patients diagnosed with Hepatitis B or C can now access medication free of charge,” Dr Amoth announced. “This initiative is a game-changer, as it will encourage early diagnosis and more effective disease management.”
He also raised concern over the high prevalence of Hepatitis C among people who inject drugs, noting that in some regions, exposure rates reach up to 25 per cent, with nearly 60 per cent of these cases progressing to chronic infection.
Dr Amoth urged continued public education, regular screening, and harm reduction strategies, particularly among high-risk populations, to curb the spread of the virus.
Top Stories Today