Only six in 10 Kenyan health facilities adequately equipped for quality care - report

The survey, which examined 3,605 facilities across all counties, including all public Level 4 and 5 hospitals, found that millions of patients, especially in rural and underserved areas, still lack access to reliable diagnostic and treatment services.
Only six in 10 health facilities in Kenya are adequately equipped to provide effective, safe and patient-centred care, a new government report has revealed, exposing major disparities in the country’s healthcare system.
The survey, which examined 3,605 facilities across all counties, including all public Level 4 and 5 hospitals, found that millions of patients, especially in rural and underserved areas, still lack access to reliable diagnostic and treatment services.
More To Read
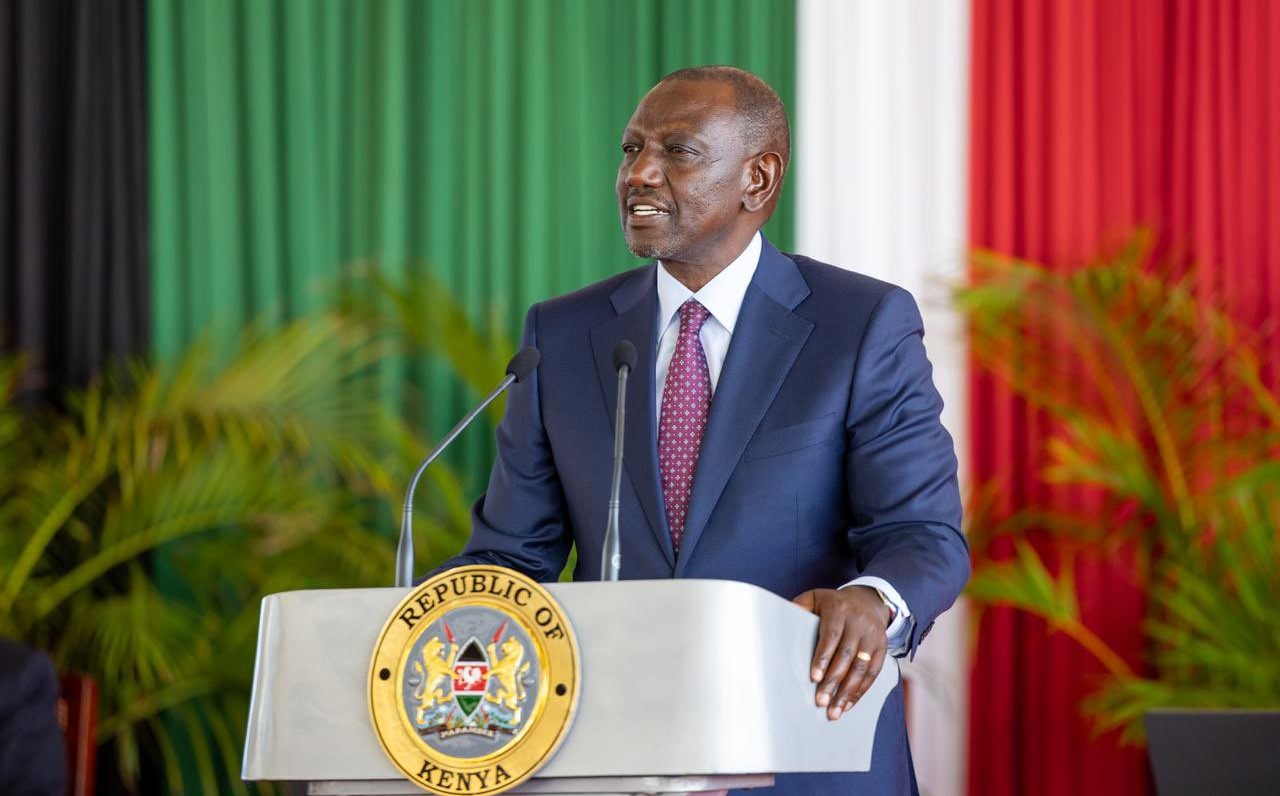
- Ruto defends health reforms, cites 27 million Kenyans registered under new coverage
- Report lays bare Kenya’s failing healthcare system
- Data gaps threaten Kenya’s health goals as key indicators on mental health, drugs go unmeasured
- MPs slam Ministry of Health over SHA failures, demand urgent reforms
- Governors, Ministry of Health, resolve to verify all UHC staff before transfers
- MPs demand urgent talks between SHA and healthcare providers over transition bottlenecks
According to the 2024 Kenya Health Facility Assessment: Quality of Care and Human Resources for Health Report, launched by Health Cabinet Secretary Aden Duale, 41 out of 47 counties have urgently requested laboratory equipment through the National Equipment Service Programme (NESP), leaving thousands of patients without access to vital medical tests.
NESP, which succeeded the Medical Equipment Service programme after its expiry in December 2023, runs on a Fee-for-Service model where vendors provide, maintain and upgrade medical equipment at no upfront cost to county governments.
Health Ministry Director General Patrick Amoth said the report revealed significant differences in quality across various types of facilities.
“The Structures Index, which quantified the extent to which health facilities are equipped with necessary building blocks to enable delivery of effective, safe, and patient-centred care, was 61 per cent,” Amoth said.
“Generally, hospitals and faith-based organisations or NGO facilities had higher scores compared to primary level and public facilities.”
The Process Index, which measures the extent to which facilities adhere to standardised, evidence-based clinical and administrative procedures, also stood at 61 per cent, with hospitals and private facilities outperforming Level 2 and 3 public facilities.
Quality improvement teams were found in 92 per cent of Level 5 facilities, 85 per cent of Level 4 facilities, and 63 per cent of Level 3 facilities. Rural facilities performed worse at 62 per cent compared to 76 per cent in urban areas. Nationally, 20,044 health workers have been trained on quality improvement initiatives over the past two years, with 25 per cent drawn from Level 5 hospitals.
The report also highlights major weaknesses in patient safety systems. Overall, death reviews were conducted in 73 per cent of facilities, but surgical death monitoring was only at 34 per cent. Maternal and perinatal death reviews performed better at 84 per cent.
“Surgical adverse events—deaths and infections within 24 hours of surgery—are at 28 per cent. The infection rate for all eight antimicrobial-resistant priority pathogens examined stood at nine per cent,” Amoth said.
However, antimicrobial resistance monitoring remains low. Only 38 per cent of facilities tracked antibiotic use, 32 per cent conducted prescription audits, and more than half, 56 per cent, did not carry out surveillance for World Health Organisation (WHO) priority pathogens.
All Level 5 facilities conducted formal death reviews, compared to 58 per cent of Level 2 facilities. Public facilities performed better at 96 per cent, while private facilities recorded 64 per cent.
Out of 427 maternal deaths reported between October and December 2023, 98 per cent were audited. Of 4,094 neonatal deaths recorded during the same period, 76 per cent were reviewed.
Only 35 per cent of facilities conducted surgical-related death reviews, with private facilities leading at 45 per cent compared to 24 per cent in public facilities. Among Level 5 facilities, 83 per cent reviewed surgical deaths, compared to 51 per cent at Level 4 and 22 per cent at Level 3.
Just 28 per cent of facilities offering inpatient services had systems to monitor surgery-related adverse events, 83 per cent of Level 5 facilities compared to only 18 per cent of Level 2 facilities. NGO facilities led at 55 per cent, while public facilities followed at 25 per cent.
Kajiado County topped the list at 90 per cent, followed by Bomet at 66 per cent. Alarmingly, no facilities in Tana River County had systems to monitor surgery-related adverse events.
Only 26 per cent of facilities conducted surveillance for patient safety incidents, with Level 5 facilities performing best at 65 per cent. Medication errors were the most monitored at 74 per cent, while blood transfusion errors were the least tracked at 14 per cent. Health worker safety surveillance was implemented in only 24 per cent of facilities.
The report further shows that medical officers accounted for four per cent of staff, general clinical officers 13 per cent, registered nurses 28 per cent, enrolled nurses five per cent, specialists (medical officers, clinical officers and nurses) three per cent each and laboratory staff 10 per cent.
Most health workers (67 per cent) were diploma trained, 13 per cent held undergraduate degrees, and eight per cent had certificates. Employment terms showed 49 per cent on a permanent basis, 33 per cent on a contract and 13 per cent under other arrangements.
Only 63 per cent of facilities had routine performance review processes. Bomet led at 96 per cent, followed by Kajiado at 91 per cent and Laikipia at 90 per cent. Marsabit had the lowest score at 20 per cent, followed by Lamu (30 per cent) and Embu (36 per cent).
Seventeen per cent of health workers reported having been assaulted, either physically or verbally, with 77 per cent of the cases involving patients and 22 per cent by caregivers. Busia County recorded the highest assault rate at 33 per cent.
Despite the challenges, 68 per cent of staff felt that workloads were fairly distributed, 85 per cent received salaries on time, but only 21 per cent had been promoted in the last three years.
The assessment also examined patient feedback, particularly on family planning services. Almost all clients (98 per cent) said they were treated with courtesy, while 90 per cent were allowed to ask questions.
“Eighty-two per cent of family planning clients nationally received their preferred method, while 15 per cent felt coerced to take another method,” Amoth said.
“Ninety-five per cent felt their choices were considered, and 87 per cent were informed about common side effects.”
Health CS Aden Duale said the assessment aims to close the gap between high service coverage and the slower improvement in health outcomes.
“Despite strides in skilled birth attendance, antenatal care and childhood vaccinations, Kenya faces persistent challenges, high maternal and childhood mortality rates, stagnant infant and neonatal death declines, and rising non-communicable diseases,” he said.
“This report presents findings of the Harmonised Health Facility Assessment conducted in Kenya, a comprehensive evaluation aimed at understanding the availability and quality of healthcare services. The assessment was initiated to generate accurate data to inform policy decisions and improve healthcare delivery.”
Duale emphasised that the findings will be used as a critical tool for policymakers, health administrators and stakeholders to identify gaps in service delivery and improve outcomes.
“The findings are based on rigorous data collection and analysis, reflecting experiences and perspectives of county managers, healthcare providers and patients alike,” he said.
“We believe this information will contribute to strategic planning, guiding us toward a healthier future for all Kenyans. Together, we can build a healthcare system that is not only accessible and affordable but also of the highest quality.”
Top Stories Today