Hormonal contraceptives linked to higher breast cancer risk, study finds

Recent studies show a small but measurable increase in breast cancer risk for women using hormonal contraceptives, highlighting the importance of informed choices.
Growing evidence suggests that hormonal contraceptives may slightly increase the risk of breast cancer, one of the leading causes of cancer-related deaths among women in Kenya.
A large study published in JAMA Oncology followed over 2 million women aged 13 to 49, tracking more than 21 million person-years. The research found that women using hormonal contraceptives—especially those with higher levels of progestin—had a higher incidence of breast cancer compared with non-users.
More To Read
- Viral infections linked to higher risk of heart attacks and strokes
- Study finds new gene-silencing therapy cuts cholesterol by 50 per cent
- How one doctor’s breast cancer battle became a message of hope for Kenyan women
- Neurological disorders on the rise in low-and middle-income countries, warns WHO
- Cardiac arrest explained: The 'silent killer' reportedly behind Raila Odinga's death
- Experts warn men are overlooking breast cancer risk
Hormonal contraceptives use synthetic forms of the natural female hormones estrogen and progesterone. Progesterone is called a progestin when manufactured synthetically.
These contraceptives prevent pregnancy in multiple ways: they stop ovulation, thicken cervical mucus to make it harder for sperm to reach an egg, and thin the uterine lining to reduce the chances of implantation.
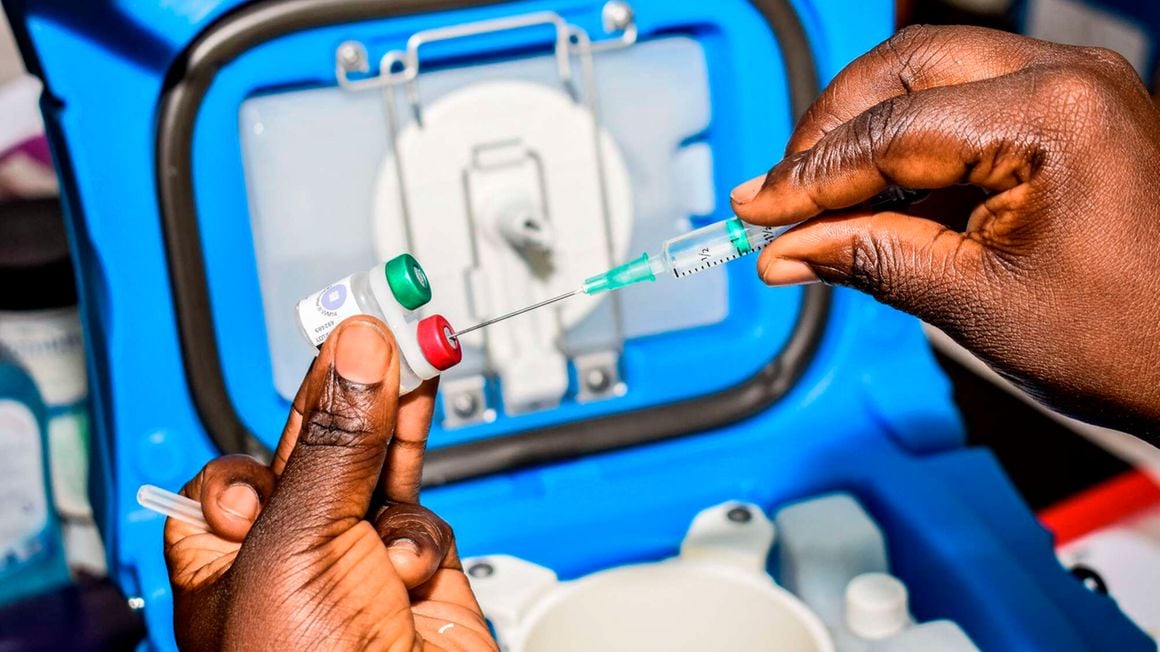
Types of hormonal contraceptives
There are several types of hormonal contraceptives. The most common are oral contraceptive pills, which come in combined formulations (estrogen and progestin) or progestin-only “mini-pills,” such as desogestrel and norethindrone.
Other hormonal methods include injections, vaginal rings, patches, and hormonal intrauterine devices (IUDs), which deliver hormones through the skin or vaginal lining, providing alternatives to daily pills.
The study showed that women using hormonal contraceptives face a slightly higher risk of developing breast cancer. The risk increase is about 12 per cent for combined estrogen–progestin pills and roughly 21 per cent for some progestin-only pills like desogestrel.
Significant at population level
This translates to around 13 extra cases of breast cancer per 100,000 women each year among users. While small for an individual, the number is significant at the population level, given the millions of women worldwide using these medications.
Breast cancer develops due to a combination of genetic, hormonal, and environmental factors. Key risk factors include inherited mutations like BRCA1 and BRCA2, prolonged estrogen exposure, ageing, obesity, alcohol consumption, smoking, and radiation exposure.
The study suggested that women who had ever used hormonal contraceptives had a 24 per cent higher relative risk of developing breast cancer compared with women who had never used them.
Progestin-only pills carried a slightly higher risk than combined pills, and desogestrel-containing pills had a higher risk than levonorgestrel-based pills.
Widely used
Hormonal contraceptives are widely used not only for pregnancy prevention but also for regulating menstrual cycles, treating acne, and alleviating endometriosis symptoms.
Despite the small increase in relative risk, the public health impact is significant due to the large number of users.
It is important to note that the study was observational, meaning it can show an association between contraceptive use and breast cancer risk but cannot prove causation.
Most women using these medications will not develop breast cancer as a result. The study also found that longer durations of contraceptive use were linked to a higher risk; for women using hormonal contraceptives for five to ten years, the hazard ratio was about 1.34.
Invasive breast cancer
A second major investigation by researchers at the University of Oxford, published in PLOS Medicine in 2023, analysed health data from 9,498 women under 50 diagnosed with invasive breast cancer and compared them with 18,171 women without the disease.
This study included a wide range of modern contraceptive methods—combined and progestin-only pills, injections, implants, and hormonal IUDs—and found a small but consistent increase in breast cancer risk for users of any hormonal contraceptive. The odds ratio was 1.23 for combined pills and 1.26 for progestin-only pills.
While relative risk was similar across contraceptive types, absolute risk varied by age. For women aged 16–20, there were about 8 additional cases per 100,000 users over 15 years, while women aged 35–39 faced around 265 additional cases per 100,000 users. The study also confirmed that the elevated risk decreases after stopping contraceptives.
Modest increase
The research underscores that the increase in breast cancer risk from hormonal contraceptives is modest, and the absolute risk for an individual woman remains low.
Hormonal contraceptives continue to provide important benefits, including reliable pregnancy prevention, menstrual regulation, acne treatment, and reduced risk of ovarian and endometrial cancers.
The findings highlight the importance of informed, individualised decisions, particularly for women with additional risk factors such as family history or BRCA gene mutations.
Globally, breast cancer remains the most common cancer among women. In 2022, around 2.3 million women were diagnosed, and approximately 670,000 died from the disease.
Incidence and mortality
The World Health Organisation warns that, if current trends continue, incidence and mortality could rise by 40 per cent by 2050. Survival rates vary widely, from over 90 per cent in high-income countries to only 40 per cent in parts of sub-Saharan Africa.
In Kenya, breast cancer is the most frequently diagnosed cancer among women and the leading type overall. In 2020, there were about 6,799 new cases, accounting for roughly 16 per cent of all new cancer cases.
Unlike many Western countries, breast cancer in Kenya often affects women at a younger age, typically between 35 and 50, and many cases are diagnosed at advanced stages, lowering survival rates.
About 68 per cent of women are diagnosed at stage III or IV, with urban counties like Nairobi reporting the highest number of cases.
Hormonal contraceptives are the most preferred method among many women due to accessibility. If these findings hold, millions could be at risk. As of 2022, about 57 per cent of married women in Kenya were using modern contraceptives.
By 2024, approximately 6.43 million women in the country were using modern methods, with around 1.9 million new users, representing a roughly 12 per cent increase from the previous year.
Among these, injectables are most popular, followed by implants, pills, and IUDs. Despite high uptake, about 14 per cent of women still have an unmet need for family planning.
Usage
Globally, in 2021, around 966 million women aged 15–49 used some form of contraception, with approximately 874 million using modern methods. Usage varies by region, with roughly 50 per cent of women in Africa using modern methods, compared to over 80 per cent in parts of Europe, Southern and Southeast Asia, and Oceania.
Hormonal contraceptives—including pills, injectables, implants, and hormonal IUDs—comprise a significant portion of modern contraceptive use in Kenya and worldwide.
Their widespread adoption highlights the importance of understanding both benefits and potential risks, including the small but measurable association with breast cancer identified in recent research.
While generally safe, hormonal contraceptives can slightly increase the risk of blood clots, stroke, or heart attack, particularly in smokers or women over 35. Users may also experience mood changes, headaches, breast tenderness, or irregular bleeding.
Top Stories Today