Health Ministry to conduct fresh staff interviews to curb fraud in new medical scheme
The decision follows concerns about the long-standing fraudulent activities within the National Health Insurance Fund (NHIF), which SHA replaced.
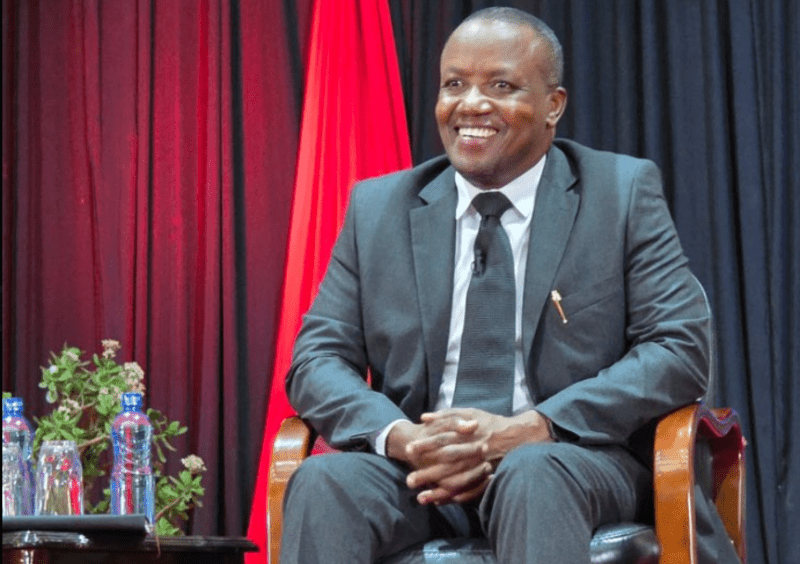
The Social Health Authority (SHA) will conduct new staff interviews to eliminate any cases of fraud within its operations, Acting Chief Executive Officer Elijah Wachira has announced.
The decision follows concerns about the long-standing fraudulent activities within the National Health Insurance Fund (NHIF), which SHA replaced.
More To Read
- SHA board names 23 assistant directors following competitive recruitment process
- Four suspects arrested for defrauding man of Sh251,000 in fake SHA registration scheme
- Five charged with defrauding Social Health Authority of Sh17.5 million
- Ministry of Health confirms maternal deaths in Kiambu, contradicting Wamatangi’s claims
- Ex-SHA bosses among nine arrested as DCI cracks down on Sh17 million health fund scandal
- Duale explains shift from Linda Mama to maternal package under SHA
Speaking during an interview with Citizen TV on Wednesday, Wachira acknowledged NHIF’s past struggles with fraud but emphasised that the cases were investigated, and staff found guilty were dismissed.
“In NHIF, when a fraud case was discovered, it was investigated, and any staff found culpable was dismissed. Therefore, many of the employees currently at NHIF were not involved in fraudulent activities,” Wachira said.
However, he explained that to ensure transparency, the SHA would be conducting fresh interviews for all staff members.
"The SHIF Act that formed SHA specifies that SHA will interview afresh its staff, and part of the interview process will of course be to check for fraud history," he added.
Principal Secretary for the State Department for Medical Services Harry Kimtai echoed Wachira’s sentiments, stating that one of the major objectives of the new registration process is to ensure clean data for every employee.
Kimtai also acknowledged the widespread fraud that plagued NHIF, saying, “The challenge that NHIF faced was fraud. Kenyans were contributing to their medical insurance cover, but a few hospitals and individuals were defrauding them, making it difficult for NHIF to improve its services."
Kimtai further explained that SHA has digitized its systems to prevent such issues.
"We have digitized the SHA system from end to end. This time, we’ve come in with regulations and laws to protect Kenyans’ investments in healthcare. Let us trust the system because we all knew, and it was you Kenyans who said that NHIF had a lot of problems," he said.
He noted that the Ministry would also be using Artificial Intelligence to detect fraud. Kimtai decried that prosecuting fraud cases in NHIF was difficult since most of the doctors or hospitals were perpetuating fraud were still open.
“That's why we made sure that we tightened our laws so that those who perpetrate fraud will never benefit from member contributions. This time, we will be able to check fraud at an early stage, and we are going to use AI to help detect it,” he said.
Top Stories Today














































