Experts urge accountability in healthcare billions to ensure Kenyans get quality services

Beyond Kenya, experts at the conference emphasised the need for African nations to develop self-sustaining healthcare financing strategies rather than relying on unpredictable donor funding.
Despite Kenya generating 85 per cent of its healthcare funding domestically, critical shortages in essential medicines and declining service quality persist.
During the Regional Health Promotion Conference last Wednesday, healthcare experts and policymakers raised concerns over these ongoing challenges in healthcare financing. They are now calling for greater transparency, accountability and efficient resource management to ensure that healthcare funds effectively translate into quality services for all Kenyans.
More To Read
- Poor remuneration pushing Kenya's community health promoters to the edge
- Financial gaps threaten Kenya's healthcare goals – DP Kindiki
- Boost for KMTC as President Ruto announces Sh600 million funding for staff recruitment
- Ministry of Health under scrutiny over Sh24 billion community health kits deal
While the common narrative suggests that Kenya relies heavily on donors for healthcare financing, the truth is that 85 per cent of its healthcare funding is generated domestically and only 18 per cent comes from donor aid. This means Kenya is largely self-reliant. This challenges the widespread belief that drug shortages stem from a lack of external funding.
Dr Abraham Rugo, the executive director of Bajeti Hub, emphasised that while Kenya largely funds its healthcare system, corruption and financial mismanagement continue to cripple service delivery.
“If Kenya is funding 85 per cent of its healthcare needs, why are patients still unable to access life-saving medications? Where is the money going?” Rugo wondered.
He pointed out that counties allocate 23-30 per cent of their annual budgets to healthcare, yet this funding remains inadequate. Despite primary healthcare facilities accounting for 90 per cent of the system, Sh120 billion — nearly 10 per cent of the total healthcare budget — is directed toward referral hospitals, leaving primary healthcare centres underfunded.
Rugo raised concerns over the Sh104 billion spent on implementing the Social Health Authority (SHA) system, arguing that these funds could have been used to upgrade existing healthcare infrastructure instead.
Corruption
“The problem with NHIF was never the system itself — it was corruption. The government chose to dismantle it rather than fix it. If we continue losing nearly 30 per cent of our healthcare budget to corruption, it is ordinary Kenyans who will suffer the most. We must hold leaders accountable.”
Dr Dickson Mwakangalu, the head of health, nutrition and WASH at Brac International, warned that without increased investment, Kenya’s goal of universal healthcare access will remain unattainable.
“Primary healthcare facilities, which serve 90 per cent of Kenyans, are operating with severe resource shortages. Community health promoters (CHPs), who are crucial for delivering healthcare services, often work without basic supplies. Some don’t even have paracetamol for their patients,” he stated.
Moses Mokua, representing the Faith-Based Service Consortium, echoed similar concerns, pointing out that Kenya’s Universal Health Coverage (UHC) programme still heavily relies on cost-sharing mechanisms, making healthcare unaffordable for many.
“Only Sh6 billion has been allocated to primary healthcare, yet it accounts for 90 per cent of our healthcare facilities. To function properly, it needs at least Sh18 billion. Instead, we have spent Sh104 billion on the SHA system, which was not even legally procured. That money could have cleared NHIF’s debt and upgraded our facilities. If we don’t closely monitor healthcare spending, SHA could become an even bigger financial burden.”
Greater funds accountability
He further demanded greater accountability for collected healthcare funds, questioning why essential services continue to be underfunded despite the government’s large financial commitments to healthcare reforms.
Beyond Kenya, experts at the conference emphasised the need for African nations to develop self-sustaining healthcare financing strategies rather than relying on unpredictable donor funding. They suggested initiatives such as health bonds and increasing reliance on domestic revenue streams to secure long-term healthcare stability.
“We cannot rely entirely on donor-funded vaccines and essential medicines. If we fail to develop sustainable solutions, we risk facing a healthcare disaster. The US does not owe us healthcare support —we do not pay their taxes,” an expert remarked.
Donne Cameron, Co-CEO of Voluntary Service Overseas (VSO), emphasised the importance of government transparency in winning public trust for UHC initiatives.
“When people understand how healthcare funds are utilised and when governments operate transparently, it becomes easier for communities to engage and support UHC efforts.”
With donor funding declining, including cuts from USAID, Cameron stressed the urgency of establishing transparent leadership and actively involving communities in decision-making processes.
Public Health Principal Secretary Mary Muthoni acknowledged concerns about healthcare financing and assured Kenyans that the government is reviewing internal funding mechanisms to prioritise critical areas.
Medical supplies
“We must ensure essential medical supplies and equipment are available at all levels — not just cut funding. While SHA has its challenges, that doesn’t mean we miscalculated. We are actively listening to concerns and working to improve the system.”
She highlighted ongoing efforts to review healthcare tariffs, especially for oncology and dialysis services, and to tackle misdiagnosis concerns through AI integration in healthcare.
A recent report by Auditor-General Nancy Gathungu has uncovered alarming levels of financial mismanagement in the Ministry of Health, revealing that millions of shillings’ worth of medical equipment and infrastructure remain idle across various counties. This has raised fresh concerns about the misuse of public funds and inefficiencies in healthcare resource allocation.
Corruption remains a persistent issue, with the NHIF being a prime example of systemic fraud. The fund was crippled by massive corruption, including fraudulent claims that led to losses exceeding Sh21 billion and administrative errors—such as typing mistakes—that cost taxpayers Sh368 million.
Despite these revelations, accountability gaps remain unaddressed, raising doubts about whether the newly introduced SHA can bridge these systemic inefficiencies, especially given its turbulent rollout.
Amid growing concerns over mismanagement, senators are demanding a full audit and overhaul of the Ministry of Health’s multi-billion-shilling budget. They cite wasteful spending, duplication of allocations, and financial mismanagement as key issues that require urgent intervention.
Intense scrutiny
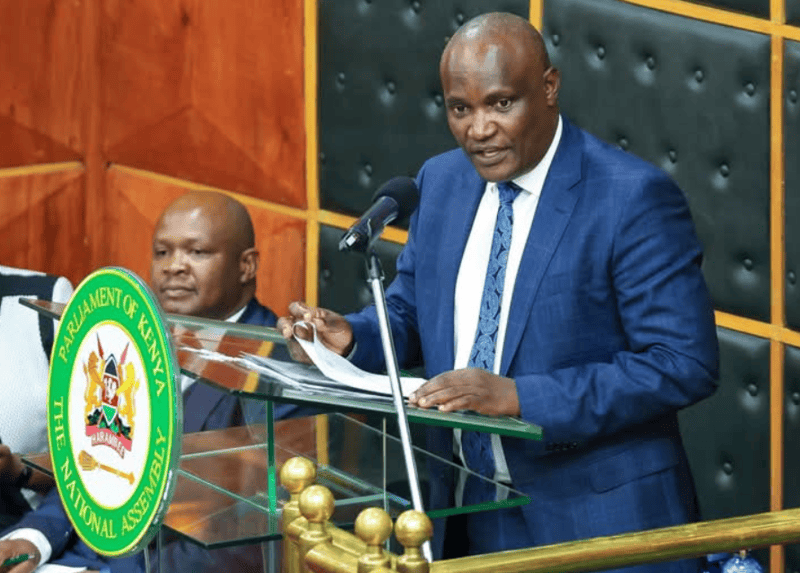
During a tense session at Parliament Buildings, Health Cabinet Secretary Debora Barasa and Principal Secretaries Harry Kimtai (Medical Services) and Mary Muthoni (Public Health) faced intense scrutiny from senators, who demanded the immediate release of Sh3.4 billion to recruit over 8,000 universal health coverage workers. The legislators also criticised questionable budget allocations, including Sh990 million for health facilities and Sh29 billion for county-level projects — funds directed by presidential orders. These allocations sparked outrage over their perceived imbalance and lack of transparency.
One of the biggest concerns raised was the sharp rise in recurrent expenditure. The budget for the State Department of Medical Services saw an astronomical increase of 98 per cent in a single year, jumping from Sh91 billion to a proposed Sh350 billion.
Senators highlighted glaring disparities in funding distribution, noting that Uasin Gishu received Sh700 million, while Turkana was allocated only Sh70 million.
Meanwhile, millions of shillings’ worth of medical equipment and infrastructure continue to gather dust in various counties, further exacerbating concerns about wasteful expenditure.
With corruption and inefficiencies draining Kenya’s healthcare system, experts and legislators are calling for greater transparency, accountability, and better resource management to ensure public funds truly benefit citizens.
Top Stories Today