Mpox could spread into conflict zones in East Africa – how to manage the response

The outbreak was declared a public health emergency of international concern by the Africa Centres for Disease Control and the World Health Organisation in August 2024.
Kenya, Rwanda, Burundi and Uganda are some of the East African countries that have reported cases of mpox – a viral infectious disease – in the latest outbreak which started in the Democratic Republic of Congo in January 2023.
The outbreak was declared a public health emergency of international concern by the Africa Centres for Disease Control and the World Health Organisation in August 2024.
More To Read
- England confirms new mpox strain: What you need to know
- Two new Mpox cases confirmed in Kenya, including patient who recently returned from South Sudan
- Mpox detected in Garissa, patient isolated as officials trace contacts
- Mpox cases in Africa surpass 190,000, deaths near 2,000: Africa CDC
- Mombasa County's mpox cases rise to 182 as health authorities activate emergency operations
- Kenya battles rising mpox infections as WHO lifts global emergency
There is a danger of the virus spreading further afield. The most vulnerable are countries in East Africa and the Horn that are at war or have recently faced serious conflicts.
Past – or ongoing – conflicts have devastated healthcare systems. Armed conflicts affect the entire spectrum of healthcare. This includes health promotion, prevention, testing, diagnosis, linkage, treatment, and follow-up.
For example, in Sudan, where conflict has raged for more than a year, 70 per cent of health facilities have been closed. What’s left of the health system is plagued by armed attacks, power outages and shortages of medical supplies and personnel.
Another country in East Africa that’s endured conflict for decades is Somalia, with devastating consequences for healthcare. It has one of the lowest coverage rates for childhood immunisation in the world.
Ethiopia is another country in the sub-region that has faced recent conflict. This is the healthcare system we have studied.
Our research focus is public health, including the negative impacts of conflict on health outcomes. We mapped the repercussions of the war in the Tigray region of Ethiopia which started in 2020. Our main findings were that medical and humanitarian services were in a state of siege. There was also evidence of a rise in illnesses.
We concluded from our research that the war had left a catastrophic humanitarian crisis, including a collapse of the healthcare system.
Insights from this as well as other research we have done in the region show clearly that armed conflict and the recent mpox outbreak make a deadly mix. And that particular steps need to be taken to manage the spread of the disease in these environments. These include collaboration with local communities and humanitarian organisations to facilitate vaccination drives. They also include engaging with military and security personnel for passage and access.
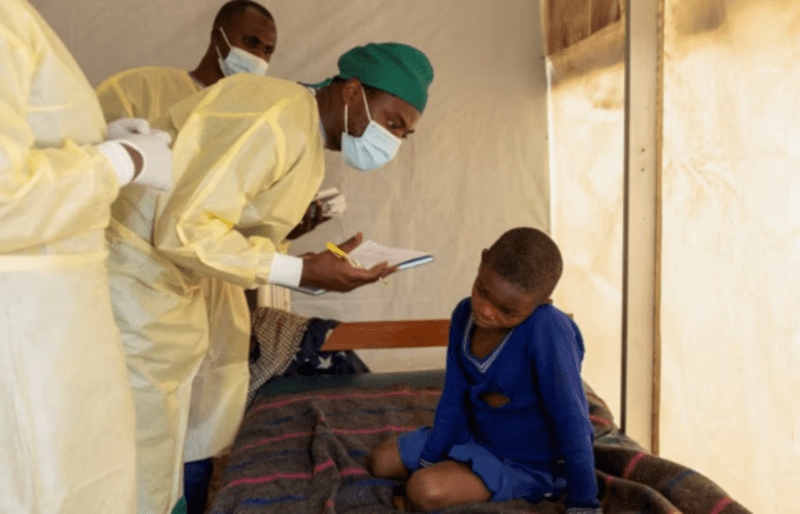 Dr. Tresor Wakilongo, verifies the evolution of skin lesions on the ear of Innocent, suffering from Mpox - an infectious disease caused by the monkeypox virus that sparks off a painful rash, enlarged lymph nodes and fever; at the treatment centre in Munigi, following Mpox cases in Nyiragongo territory near Goma, North Kivu province, Democratic Republic of the Congo July 19, 2024. (Reuters)
Dr. Tresor Wakilongo, verifies the evolution of skin lesions on the ear of Innocent, suffering from Mpox - an infectious disease caused by the monkeypox virus that sparks off a painful rash, enlarged lymph nodes and fever; at the treatment centre in Munigi, following Mpox cases in Nyiragongo territory near Goma, North Kivu province, Democratic Republic of the Congo July 19, 2024. (Reuters)
Finally, it’s important to factor in vaccinations for people in transit and those crossing borders, as well as refugees and people living in internally displaced camps.
What we can learn from the Tigray crisis
The civil war in Tigray that lasted from November 2020 to November 2022 involved the federal government of Ethiopia imposing a blockade on the entire region.
This caused a collapse of the entire healthcare system – and a humanitarian crisis.
Our research, published in 2021, found evidence of forced displacement of two million people, deliberate damage of 70 per cent - 80 per cent of health facilities, targeted attacks on health workers, and rape of women and girls.
A second study in which the lead author of this article was involved surveyed 4,381 children under the age of one to investigate the impact of the armed conflict on the use of child health services in Tigray. The survey found that 39 per cent of infants received no basic vaccines, 61.3 per cent of the children under the age of one received at least one vaccine, and 20 per cent received all the vaccinations recommended for their age.
 A child suffering from mpox at a hospital isolation unit in South Kivu province. (UNICEF)
A child suffering from mpox at a hospital isolation unit in South Kivu province. (UNICEF)
Our findings on the impact of conflict on vaccine rollouts were echoed in a recent WHO report which found that 12 of the 18 states of Sudan are simultaneously experiencing three or more outbreaks of infectious diseases such as cholera, dengue, malaria, measles, suspected pertussis and meningitis.
What this means for containing the spread of mpox
Armed conflict deters health promotion and prevention activities, increases the transmission of outbreaks, collapses healthcare services, and affects vaccine rollout such as mpox vaccine. Vaccines are vital to limiting the severity of the illness and halting the outbreak.
Africa CDC has pledged to deliver 10 million mpox vaccine doses by 2025. Two million of these will be delivered in 2024 with the goal of equitable vaccine access across African nations. But, even if these vaccines are made available, ongoing conflicts or fragile stability are likely to get in the way of delivery.
We suggest the following steps could help mitigate this.
1. Coordinate vaccine delivery with other humanitarian aid: To efficiently use public health resources in general and mpox vaccine in particular, it is important to coordinate the delivery of vaccines with other ongoing humanitarian response activities.
2. Engage local communities: This would protect frontline workers from conflict and improve trust in the vaccine itself. Most importantly, the engagement is crucial to establishing permanent vaccination teams from local communities.
3. Collaborate with military and security personnel: It may be important to arrange military escorts during the delivery of vaccines as has been done for humanitarian aid in conflict settings.
4. Negotiate to secure physical access: Identifying conflict actors and their allies and negotiating access is critical to reducing field operational risks and delivering mpox vaccine.
5. Transit and cross-border vaccination: Forced population displacement is a common feature of conflict settings, so it may be helpful to deliver vaccines at the transit points.
6. Vaccine delivery where people are sheltered: It is also important to plan to deliver the vaccine at the refugee and internally displaced person camps.
Top Stories Today