Sleep apnea: The silent threat to brain health and cognitive brain function

Addressing lifestyle factors, using medical devices, or opting for surgical interventions can help manage the disorder and improve overall health.
A recent study published in Neurology, the medical journal of the American Academy of Neurology, has revealed a significant connection between sleep apnea and neurological diseases that impair cognitive brain function.
Sleep apnea, a serious sleep disorder where breathing repeatedly stops and starts during sleep, disrupts oxygen flow to the brain and body. This condition has already been associated with health issues such as Alzheimer's disease, dementia, obesity, and high blood pressure.
More To Read
- How maternal and neonatal health could determine dementia risk decades later
- Medical cannabis under scrutiny as new evidence highlights limited benefits and real risks
- Why smartphones before age 12 raise risks of depression, obesity and poor sleep
- The hidden connection between snoring, interrupted sleep and rising global Parkinson’s epidemic
- Study flags stark inequities in global epilepsy care, medication
- Study suggests adolescence may last until age 32
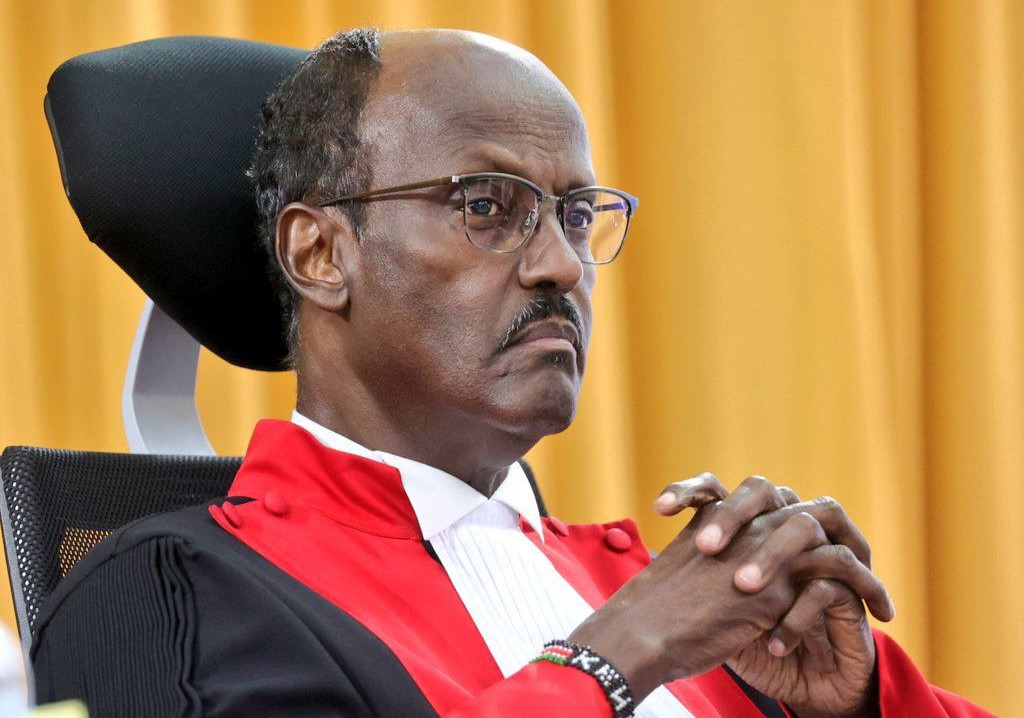
The study, led by Dr Ramos, specifically focused on older adults of Latin descent. About 2,600 Latino participants with an average age of 68 were recruited.
The researchers aimed to explore why Latinos face an increased risk of Alzheimer’s disease compared to other ethnic groups, a disparity not fully explained by known risk factors.
“Latinos have a higher prevalence of sleep apnea, and examining markers of brain health in this population helps identify early indicators of disease risk for Alzheimer’s and overall brain health,” Ramos explained.
At the study's start, participants underwent a home-based sleep test measuring breathing disruptions, shallow breathing, and blood oxygen levels during sleep. Based on the results, participants were categorised into three groups:
-Those with fewer than five sleep disruptions per hour or no sleep issues.
-Those with five to 15 disruptions, indicating mild sleep problems.
-Those with more than 15 disruptions, classified as moderate to severe difficulties.
Key findings on brain health
After 10 years, participants underwent brain scans to measure brain volume and assess white matter damage. White matter, which naturally declines with age, plays a critical role in brain connectivity.
The study found that participants with the most significant sleep issues had a 0.24 cm³ greater hippocampal volume compared to those with no sleep problems. Furthermore, for each additional sleep disruption, there was an increase of 0.006 cm³ in hippocampal volume. However, this increase in size is thought to reflect swelling caused by inflammation or damage rather than healthier brain function.
Researchers estimate that approximately 936 million adults worldwide suffer from sleep apnea.
Past studies have shown that sleep apnea increases the risk of several conditions, including obesity, type 2 diabetes, and high blood pressure. Of particular concern is its link to neurological disorders such as Alzheimer’s disease and other forms of dementia.
Dr Alberto R. Ramos, a professor of clinical neurology and research director at the Sleep Medicine Programme at the University of Miami, highlighted the importance of addressing this condition.
“Sleep apnea is still an under-recognised and undertreated sleep disorder that can affect brain and cardiovascular health. If sleep apnea impacts brain health and increases dementia risk, its treatment could be a strategy to improve brain health and prevent these disorders, which are on the rise,” said Ramos.
Oxygen levels and white matter damage
Lower oxygen levels during sleep were linked to higher hippocampal volume and more extensive white matter hyperintensities — areas of brain damage associated with vascular brain disease.
“These findings suggest that vascular brain disease in people with sleep apnea is partially explained by the low oxygen levels characteristic of this condition,” Ramos noted.
While treatment studies are still needed, addressing sleep apnea could mitigate early markers of diseases like dementia and vascular brain disease.
“The changes leading to dementia often begin decades before clinical symptoms appear,” Ramos said.
“Identifying the role of sleep apnea in this process could open pathways for early interventions.”
By recognising and managing sleep apnea, particularly in high-risk populations, researchers hope to slow the progression of cognitive decline and improve overall brain health.
The National Institute of Neurological Disorders and Stroke notes that individuals with sleep apnea may partially awaken as they struggle to breathe, although they are often unaware of these disturbances when they wake up in the morning.
The most prevalent form of sleep apnea is obstructive sleep apnea (OSA), which occurs when the soft tissue at the back of the throat relaxes too much and blocks the airway. Central sleep apnea (CSA), on the other hand, results from irregular signals from the brain that fail to trigger proper breathing. Many people experience a combination of both OSA and CSA.
Excessive daytime sleepiness
A hallmark symptom of sleep apnea is excessive daytime sleepiness, but it can also manifest in other ways, including restless sleep, loud snoring interrupted by periods of silence followed by gasps, falling asleep during the day, morning headaches, difficulty concentrating, irritability, forgetfulness, and mood or behaviour changes such as anxiety and depression.
While these symptoms don’t always indicate sleep apnea, it is important to consult a healthcare provider, especially if any of these signs are present. Sleep apnea is more common in men and those who are overweight or obese.
Sleep apnea can affect anyone, but certain groups are at a higher risk. People who are at greater risk for sleep apnea include:
-Overweight or obese individuals: Excess weight, especially around the neck, can increase the likelihood of airway obstruction during sleep.
-Men: Sleep apnea is more common in men, though women can develop it too, especially after menopause.
-Older adults: The risk of sleep apnea increases with age, particularly after 50.
-People with a family history: Genetics play a role, so those with a family history of sleep apnea may be more likely to develop it.
-People with certain medical conditions: Conditions such as high blood pressure, heart disease, diabetes, and neurological disorders increase the likelihood of sleep apnea.
-Smokers: Smoking can increase inflammation and fluid retention in the upper airway, raising the risk of sleep apnea.
-People with anatomical abnormalities: Structural issues like enlarged tonsils, a thick neck, or a deviated septum can obstruct the airway during sleep.
-Those with sedentary lifestyles: Lack of physical activity can contribute to obesity, which is a significant risk factor for sleep apnea.
Treatment for sleep apnea depends on the individual’s medical history and the severity of the condition.
Initially, lifestyle changes are often recommended, such as avoiding alcohol and sedatives, losing weight, and quitting smoking.
Some individuals benefit from using special pillows or devices designed to prevent sleeping on their backs, or oral appliances that help keep the airway open during sleep.
If these conservative methods prove insufficient, doctors may suggest the use of a continuous positive airway pressure (CPAP) machine, which delivers pressurised air through a face mask to keep the airway open.
Alternative devices, such as variable positive airway pressure (VPAP) and automatic positive airway pressure (APAP) machines, are also available.
In more severe cases, surgical procedures may be considered to remove excess tissue or widen the airway.
Additionally, the FDA has approved a surgically implantable device that monitors breathing signals during sleep and stimulates a nerve to regulate breathing.
If left untreated, sleep apnea can be dangerous.
Excessive daytime sleepiness can lead to accidents, such as falling asleep while driving. Moreover, untreated sleep apnea increases the risk of stroke, transient ischemic attacks (TIAs), and a range of cardiovascular issues, including coronary heart disease, heart failure, irregular heartbeat, heart attack, and high blood pressure.
While there is no cure for sleep apnea, effective treatment can reduce the risks of heart-related complications and high blood pressure.
Sleep apnea is a serious condition that requires proper diagnosis and treatment to prevent long-term health complications.
Addressing lifestyle factors, using medical devices, or opting for surgical interventions can help manage the disorder and improve overall health.
Top Stories Today