How follow-up programmes bridge treatment gap in non-communicable diseases

As of 2024, approximately 589 million adults aged 20 to 79 are living with diabetes, which equates to roughly one in nine adults worldwide. Projections indicate that by 2050, this number could rise to 853 million.
Untreated high blood pressure has quietly become one of the most urgent health threats of our time. Often symptomless, it damages the heart, kidneys, eyes, and blood vessels long before most people realise something is wrong.
This single condition lies at the centre of many of today’s fastest-growing non-communicable diseases (NCDs), including heart disease, stroke, kidney failure, and diabetes complications. Yet despite its severity, many Kenyans remain unaware of their blood pressure status.
More To Read
- Microplastics and heart disease: Emerging evidence of a hidden cardiovascular threat
- Study shows women under 50 face higher risk of colon growths from ultra-processed foods
- Why gestational diabetes is no longer a temporary pregnancy problem
- WHO issues first global guidelines on diabetes in pregnancy
- Study links excess screen time in children to higher heart and metabolic risk
- Viral infections linked to higher risk of heart attacks and strokes
According to the Ministry of Health, hypertension affects one in four adults, with a national prevalence of 28.6 per cent. Only 29.4 per cent of individuals with hypertension know they have the condition, nearly 78 per cent of those diagnosed are not on treatment, and among the few receiving care, just 3 per cent have successfully controlled their blood pressure.
Health experts warn that closing these access gaps could be a game-changer.
To address the challenge, Boehringer Ingelheim launched a patient-focused pilot programme in 2022 in partnership with local healthcare providers, including faith-based facilities, across Kenya. The initiative integrates follow-up care, treatment adherence support, and personalised coaching to improve outcomes for individuals living with hypertension and diabetes.
Community outreach screenings identify at-risk individuals, who are then diagnosed early and enrolled in a 12-month follow-up programme. Coaching on nutrition, lifestyle modification, and access to quality healthcare and medication aims to improve disease control in underserved populations.
Follow-up is critical in managing hypertension. It ensures early detection of complications, adherence to treatment, and ongoing patient education.
Regular monitoring allows providers to adjust therapy, track progress, and support lifestyle changes, essential for preventing long-term complications such as heart disease, stroke, and kidney failure. Yet poor adherence to medication remains a major challenge, undermining outcomes and increasing risks.
Dr Rilwan Adan, head of the Lion Diabetes Centre, notes a worrying trend: many patients present with eye problems such as blurry vision, only to discover their symptoms stem from uncontrolled blood sugar.
 Dr Rilwan Adan, head of the Lion Diabetes Centre. (Photo: Charity Kilei)
Dr Rilwan Adan, head of the Lion Diabetes Centre. (Photo: Charity Kilei)
“Many people do not know they are living with diabetes or hypertension. It is a silent killer. Symptoms develop slowly, and by the time patients seek help, they may already be facing serious complications,” she says.
These complications, including heart attacks, stroke, kidney failure, blindness, and amputations, can drastically affect quality of life. Dr Adan stresses the importance of early detection as the most effective way to prevent irreversible damage.
“Our goal is to identify patients early. We conduct regular screenings, check blood sugar levels, and educate individuals so they can prevent complications.”
She adds that partnerships have boosted awareness, but adherence to long-term treatment remains difficult. Many patients stop medication once they feel better, unaware that conditions like diabetes and hypertension require lifelong management.
“We provide continuous coaching and support groups. These help patients understand their condition better and stay committed to treatment.”
Data shows a steady rise in NCDs, particularly in low-income and marginalised areas. If unmanaged, diabetes and hypertension often lead to cardiovascular disease, the leading cause of death globally and in Kenya. In many cases, the first noticeable symptom may be a stroke, kidney failure, or sudden vision loss.
Retinopathy, for example, develops silently and without pain. Some individuals only discover they have diabetes after presenting with blindness. Others face amputations or severe organ damage before diagnosis.
“All these complications affect quality of life, and many could be prevented with earlier screening and consistent follow-up,” Dr Adan emphasises.
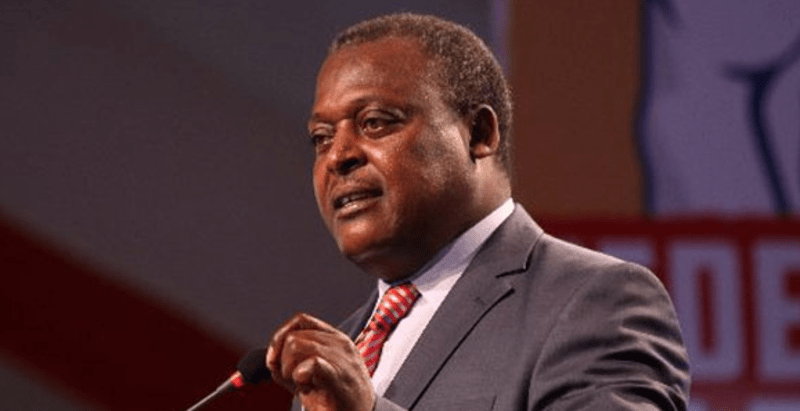
George Kuria, who oversees healthcare access for Boehringer Ingelheim in Kenya, highlights systemic gaps: limited medication availability, cost barriers, and insufficient health worker capacity.
 George Kuria. He oversees healthcare access for Boehringer Ingelheim in Kenya. (Photo: Charity Kilei)
George Kuria. He oversees healthcare access for Boehringer Ingelheim in Kenya. (Photo: Charity Kilei)
“In many communities, people struggle to access even basic treatment,” he says. “We focus on awareness and ensure that once a patient is diagnosed, they are enrolled in a structured program with ongoing support.”
The model integrates community health workers, nurses, and facility-based practitioners, ensuring patients receive guidance from trusted providers. Beyond diagnosis, patients benefit from affordable medication and a 12-month follow-up program designed to reinforce adherence.
“We have seen significant improvement,” Kuria notes. “Patients are asking questions, joining support groups, and forming networks to encourage one another. This engagement shows the approach is working.”
He adds that continuous community education is vital, particularly around diet, physical activity, and early health-seeking behaviours.
“Communities must prioritise their health. Awareness builds trust, and trust improves decisions.”
NCDs are now among Kenya’s leading killers. Hypertension claims about 5,035 lives annually, diabetes 3,822, and cardiovascular diseases 7,478.
Hale Asikoglu, Head of Sustainable Development at Boehringer Ingelheim, explains that Kenya was chosen as a pilot country for a comprehensive access program targeting underserved communities. The initiative includes prevention, consultation, referral, diagnosis, coaching, and treatment, particularly for hypertension and diabetes.
 Hale Asikoglu, Head of Sustainable Development at Boehringer Ingelheim. (Photo: Charity Kilei)
Hale Asikoglu, Head of Sustainable Development at Boehringer Ingelheim. (Photo: Charity Kilei)
Asikoglu reports strong progress: 8,400 underserved patients enrolled in structured care and over 180,000 reached through outreach.
“We guide each patient through a 12-month management journey. Mobile clinics and community screenings help us identify high-risk individuals early,” she says.
She stresses hypertension’s danger: “You cannot see it, and it doesn’t cause pain. Many patients arrive when it is already too late. Our goal is to fight this disease by ensuring people get screened before complications occur.”
She describes heartbreaking cases where patients seek care only after severe complications, and some do not survive.
“No one should die from a preventable disease,” she emphasises. “We must amplify awareness, ensure access to treatment, and support people before they get sick.”
She underscores community-driven solutions, strong partnerships, and sustained public education, noting, “We want communities to understand these conditions, recognise the risks, and feel empowered to act. With the right information and support, many illnesses can be prevented, managed, and controlled.”
The program currently operates in Nairobi, Mombasa, and other communities, with a vision to impact 50 million people worldwide.
Top Stories Today